Three years ago, I received a call at midnight from a health plan CEO whose voice was tight with stress. A CMS audit loomed in 72 hours, and his organization's provider directory was a disaster. Post-merger integration had left them with fragmented data across multiple systems, outdated provider information, and no way to verify accuracy quickly.
"Each directory error could cost us $25,000," he told me. "We've already found dozens of problems. We're facing millions in potential fines."
His team spent the next three days working around the clock, pulling staff from member services and operations just to compile basic compliance documentation. They passed the audit—barely—but the experience revealed a fundamental weakness that could cripple their growth.
Today, that same organization completes CMS audits in under two hours with zero violations. Their transformation illustrates exactly why provider directory management has become the key to differentiating between health plans that thrive and those that struggle in 2025.
Why Provider Directories Have Become Strategic Weapons
Provider directory management used to be a back-office compliance task. Now it's a competitive differentiator that determines which health plans win in the market. Three forces have converged to make this transformation inevitable:
• Regulatory Stakes Are Skyrocketing: Medicare Advantage plans face civil monetary penalties up to $25,000 per determination for directory inaccuracies. States are adding their requirements—California demands updates within 15 days, Florida has new telehealth credentialing rules, and New York requires rapid sanction reporting. The compliance burden is expanding more rapidly than most organizations can adapt to.
• Member Expectations Have Changed: Healthcare consumers now expect the same real-time accuracy they get from Google Maps or restaurant apps. When they search for a provider, they want current information about availability, location, and network status. Directory problems that once generated complaints now drive members to switch plans during open enrollment.
• Operations Have Become Complex: Health plan operations have grown exponentially more complex through mergers, acquisitions, and rapid market expansion. Managing provider networks across multiple states and systems while maintaining accuracy has become nearly impossible due to the use of manual processes.
The organizations winning in this environment have made a fundamental shift: they've moved from reactive directory management to predictive systems that prevent problems before they occur.
The Hidden Costs of Staying Reactive
Most health plans still manage provider directories the old way—updating information after problems surface, processing changes in monthly batches, and scrambling to prepare for audits.
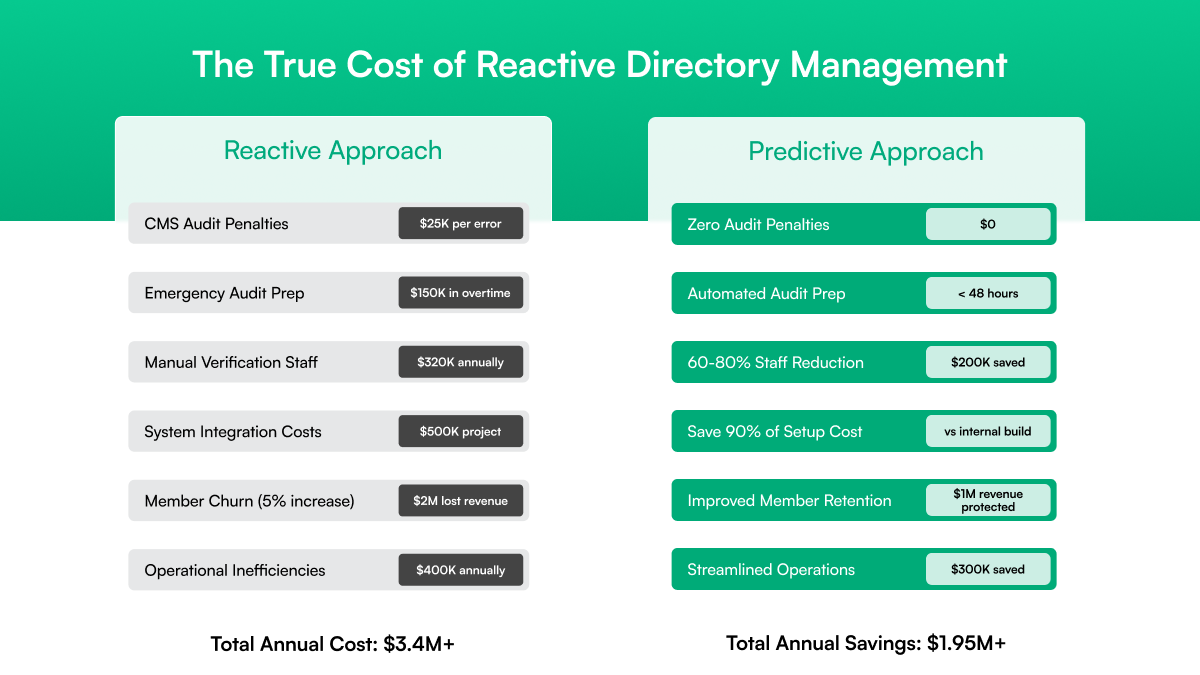
This reactive approach creates three expensive vulnerabilities:
• Data becomes fragmented and unreliable
• Manual processes create operational bottlenecks
• Compliance becomes crisis management
Let's examine how each of these vulnerabilities undermines health plan operations and creates competitive disadvantages:
Data Becomes Fragmented and Unreliable
Providers submit changes through multiple disconnected channels: phone calls, fax transmissions, email notifications, and online portals. Each touchpoint creates potential for error and delay.
Staff must manually update information across EHR systems, claims platforms, member portals, and compliance databases—often discovering discrepancies weeks or months after the updates are made.
Organizations that have grown through mergers face additional chaos. Reconciling provider networks from different systems, each with its own data formats and update processes, often reveals data quality problems that have been accumulating for years.
Manual Processes Create Operational Bottlenecks
Traditional directory management relies heavily on manual verification, which doesn't scale. Staff check provider credentials against various databases, verify license status with state boards, and cross-reference information across multiple systems.
These manual processes consume a substantial amount of time, are prone to human error, and become increasingly difficult to maintain as provider networks expand.
The Standish Group reports that 52% of healthcare IT projects exceed original budgets and timelines, making internal solutions to these problems particularly risky and expensive.
Compliance Becomes Crisis Management
Organizations using reactive approaches typically spend weeks preparing for regulatory audits, requiring staff to work overtime compiling reports and validating data accuracy.
This crisis-driven approach to compliance consumes resources that could be invested in enhancing the member experience or implementing strategic growth initiatives.
When audit preparation repeatedly disrupts normal operations, it reveals that the underlying approach to directory management is fundamentally flawed.
The cumulative effect of these vulnerabilities creates a vicious cycle: poor data quality leads to compliance problems, which consume resources that could be used to prevent future data quality issues. Breaking this cycle requires a fundamentally different approach.
How Leading Health Plans Operate Differently
The most successful health plans have completely reimagined provider directory management. Instead of reacting to problems, they prevent them through predictive systems that continuously monitor, analyze, and update provider information.
Their approach focuses on three key capabilities:
They Use Real-Time Intelligence to Stay Ahead
Leading organizations deploy platforms that integrate with authoritative data sources across all states where they operate. These systems continuously monitor license status, credential expirations, and sanction databases, identifying potential issues weeks before they affect members or compliance status.
This proactive approach enables health plans to manage credential renewals, address license lapses, and update network information before issues impact operations or the member experience. Instead of discovering problems during quarterly reviews, they receive alerts that enable them to take preventive action.
They Eliminate Data Silos Through Integration
Modern provider directory platforms provide seamless integration with existing EHR systems, claims platforms, and member portals. When provider information changes, updates are propagated across all connected systems simultaneously, eliminating the need for manual reconciliation that can create errors and delays.
This integration capability proves particularly valuable for organizations that have grown through mergers or operate across multiple markets with different systems. Instead of managing data silos that create inconsistencies, they maintain a single source of truth that all systems reference.
They Build Compliance Into Operations
Rather than treating compliance as a separate requirement, leading platforms integrate regulatory requirements into their core system architecture. This includes the generation of automated audit trails, real-time compliance monitoring, and comprehensive reporting capabilities that transform audit preparation from a crisis management task to a routine operation.
The result: audits become demonstrations of operational excellence rather than tests of crisis management capabilities.
This predictive approach represents a fundamental shift in thinking—from reactive problem-solving to proactive prevention. Organizations making this transition gain significant competitive advantages that compound over time.
Assured's Unique Approach: Why We're Different
When we built Dawn Health, we experienced these challenges with provider directories firsthand. Scaling from 0 to 150+ providers across 15 states taught us exactly where traditional approaches fall short and what health plans truly need. We built Assured to solve these problems at their source through three unique advantages:
Comprehensive Monitoring That Misses Nothing
Assured's NCQA-certified platform monitors over 2,000 authoritative data sources, including all state licensing boards, federal exclusion databases, professional certification organizations, and hospital affiliation systems.
This comprehensive coverage ensures that credential changes are identified and processed, regardless of their origin.
Our AI-powered monitoring analyzes patterns across these data sources to predict potential credential issues 30 days in advance. While generic platforms typically monitor 500-1,000 sources, our comprehensive approach provides the accuracy and reliability that health plans need to operate with confidence.
Native EHR Integration That Just Works
Unlike platforms that require months of custom development for each integration, Assured provides pre-built connectors for major EHR systems, including Epic, Cerner, Allscripts, and athenahealth.
Our integration approach enables real-time data synchronization without consuming internal IT resources or creating ongoing maintenance burdens.
When a provider's license status changes in any state, the update appears instantly across your EHR, member portal, claims system, and compliance dashboards. This eliminates the delays that create member experience problems and compliance gaps.
Implementation That Delivers Results in 2 Weeks
Most platform implementations take 6-12 months and significantly disrupt operations. Assured's proven methodology gets health plans fully operational in 2 weeks with zero compliance gaps:
Rapid Assessment and Setup (Days 1-3): We conduct a focused analysis of your current state, identifying critical integration points and highest-risk provider data. Our team works with your IT, operations, and compliance teams to configure the platform for immediate deployment.
Live Deployment with Real-Time Support (Days 4-14): Complete migration occurs with parallel operation to ensure business continuity. We provide hands-on support, real-time monitoring, and immediate optimization based on your organizational workflow requirements. This phase typically demonstrates immediate improvements in data accuracy and readiness for compliance.
This accelerated methodology has enabled successful implementations across health plans of all sizes, including organizations managing complex post-merger integrations.
The Strategic Benefits: Beyond Compliance
Organizations that implement predictive provider directory management achieve benefits that extend far beyond regulatory compliance. These strategic advantages transform how health plans compete in the market:
Operational Efficiency: Automated processes typically reduce manual workload by 60-80%, freeing staff to focus on higher-value activities such as network development and member engagement. Staff who previously spent days preparing for audits can focus on strategic initiatives that drive growth.
Competitive Advantage: Rapid provider onboarding capabilities enable faster response to market opportunities. When competitors take months to add new providers, organizations with automated systems can respond in days, capturing market share and growth opportunities.
Member Experience: Real-time directory accuracy eliminates the frustrating experiences that drive member complaints and churn. Members find accurate provider information when they need it, which supports improvements in retention and satisfaction.
Risk Management: Comprehensive compliance monitoring and automated audit preparation reduce regulatory risk while providing financial protection through vendor liability coverage.
Why Building Internal Solutions Fails
Organizations evaluating provider directory management often consider building internal solutions. Based on our experience and industry data, this approach consistently fails to deliver acceptable results for several critical reasons:
Development Costs Exceed Projections: Software developers with healthcare experience earn a median salary of $110,140, according to Bureau of Labor Statistics data, with specialists commanding additional premiums. Beyond personnel costs, development requires significant investment in cloud infrastructure, security systems, and ongoing maintenance. Gartner research indicates that annual maintenance typically accounts for 15-25% of the initial development investment.
Implementation Takes Years, Not Months: Healthcare IT projects face well-documented challenges. The Standish Group reports that 52% of healthcare IT projects exceed original budgets and timelines. Internal directory management projects typically require 18-24 months for basic functionality, with additional time needed for comprehensive compliance coverage.
Compliance Expertise Is Expensive and Hard to Retain: Maintaining compliance across 50+ state regulatory frameworks requires specialized expertise that's difficult to hire and expensive to retain. Organizations must stay current with changing requirements while building technical capabilities—a combination that proves challenging for most internal teams.
Opportunity Costs Are Hidden but Substantial: The most significant cost of internal development is the opportunity cost. Every resource invested in infrastructure development is a resource not available for core business activities, such as improving member experience, expanding the network, or implementing strategic growth initiatives.
Given these challenges, leading health plans increasingly choose specialized vendor partnerships that provide immediate access to proven capabilities.
Why Smart Health Plans Choose Specialized Vendor Partnerships
Leading health plans choose vendor partnerships for provider directory management because specialized platforms provide immediate access to capabilities that would take years to develop internally:
Immediate Access to Proven Technology: Assured's platform represents years of development and refinement, with established relationships with regulatory bodies and comprehensive compliance frameworks in place. Organizations gain immediate access to capabilities that would require substantial internal investment to replicate.
Risk Transfer and Liability Protection: Our NCQA CVO certification provides independent validation of compliance processes that individual organizations would need to develop separately. This certification also transfers compliance risk from health plans to specialized vendors with appropriate insurance coverage and financial backing.
Focus on Core Competencies: Vendor partnerships enable organizations to focus their internal resources on core competencies—such as member experience, network development, and strategic growth—while leveraging specialized expertise for infrastructure management and regulatory compliance.
Your Strategic Decision: Transform Directory Management Into Competitive Advantage
The health plan CEO who called me three years ago transformed his organization from a compliance crisis to industry leadership through strategic adoption of technology. His team now completes audits in hours instead of weeks, achieves perfect compliance records, and focuses on strategic growth initiatives instead of manual compliance tasks.
Most importantly, his organization gained the agility to respond quickly to market opportunities while competitors struggled with manual processes. When new markets open or network opportunities arise, they can onboard providers in days rather than months, capturing growth that more agile competitors would otherwise capture.
Your organization faces the same strategic opportunity. Provider directory management can remain an operational burden that consumes resources and creates compliance risk, or it can become a competitive advantage that enables rapid growth and superior member experience.
The regulatory environment will continue tightening. Member expectations will continue rising. Operational complexity will continue increasing. Organizations that act now position themselves for sustainable competitive advantage. Those who delay will find themselves fighting increasingly difficult battles with inadequate tools.
The choice is clear: transform your provider directory management into a competitive advantage, or watch competitors gain an edge that becomes impossible to overcome.
Assured's NCQA-certified platform has helped health plans across all 50 states eliminate directory management crises while improving operational efficiency and member experience.
Our comprehensive monitoring, seamless integration, and proven implementation methodology deliver results within 2 weeks.
Ready to stop fighting provider directory crises and start gaining a competitive advantage?
Contact me directly at varun@withassured.com to discuss how we can transform your provider directory management within 2 weeks.
Your next CMS audit doesn't have to be a crisis. It can be a demonstration of operational excellence that positions your organization for sustainable growth and competitive advantage.


.jpg)
.png)


.png)


