Manual provider data monitoring may seem more economical, but at scale, it’s the fastest way for your healthcare organization to face serious compliance risks and financial penalties.
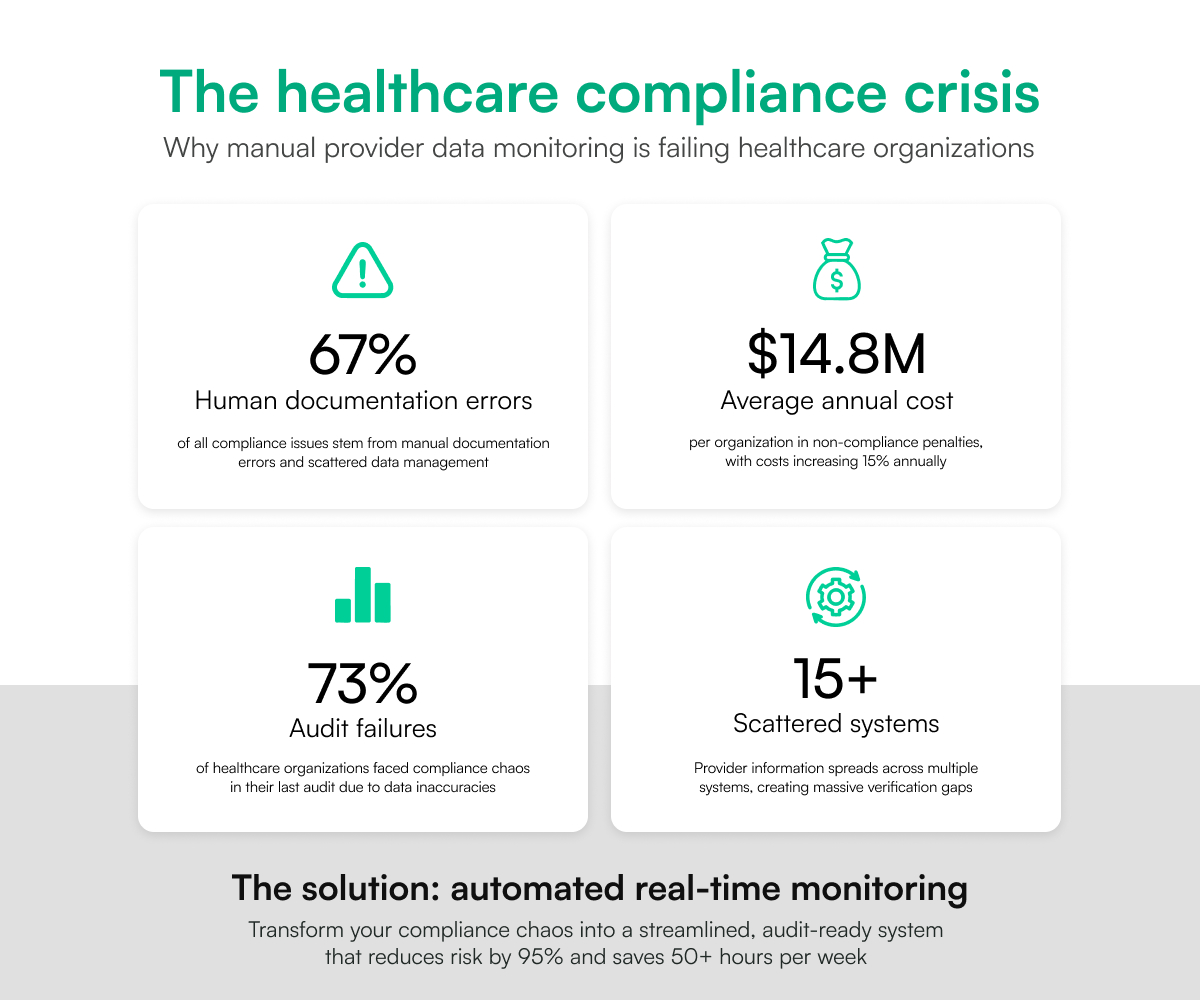
Healthcare facilities that rely on manual monitoring processes face numerous challenges. The most pressing issue is scattered data. Provider information is scattered across 15+ systems, creating huge verification gaps. Additionally, human documentation errors complicate matters and lead to 67% of compliance issues.
While organizations struggle with these challenges, stricter regulations and standards are imposed regularly by NCQA, CMS, and the Joint Commission. Non-compliance costs an average of $14.8 million annually per organization.
The word is chaos.
The result? Over 73% of healthcare organizations faced this ‘chaos’ in their last compliance audit due to provider data inaccuracies, costing huge fines and operational disruptions.
Automation offers a solution to these persistent challenges, and this guide will show you how to fix compliance issues with automated real-time monitoring.
What Real-Time Provider Data Monitoring Actually Means
Real-time provider data monitoring is simply the continuous verification of healthcare provider credentials, licenses, and compliance status across multiple authoritative sources, providing instant alerts when changes occur.
An effective real-time provider data monitoring system ensures:
- 24/7 monitoring instead of periodic checks
- Direct connections to state boards, NPPES, and DEA
- Instant notifications alerting you to status changes
- Centralized dashboard serving as a single source of truth for your entire provider network
The Technology Behind It
The API integrates with over 2,000 verification sources and utilizes AI-powered data matching and validation to provide real-time status updates and expiration tracking.
Automated real-time monitoring trumps traditional approaches because:
- Excel spreadsheets and manual tracking can't scale
- Quarterly reviews miss real-time changes
- Staff turnover disrupts institutional knowledge
- Manual processes lack a centralized source of truth
Automation ensures you stay current with credentialing, data verification, and compliance requirements while avoiding massive fines and operational disruptions.
Read on to find out how to implement automated provider data monitoring.
How to Implement Automated Provider Data Monitoring
To implement automated provider data monitoring for your organization, you need to assess your current technology, identify integration opportunities, and train your staff to manage the new system effectively.
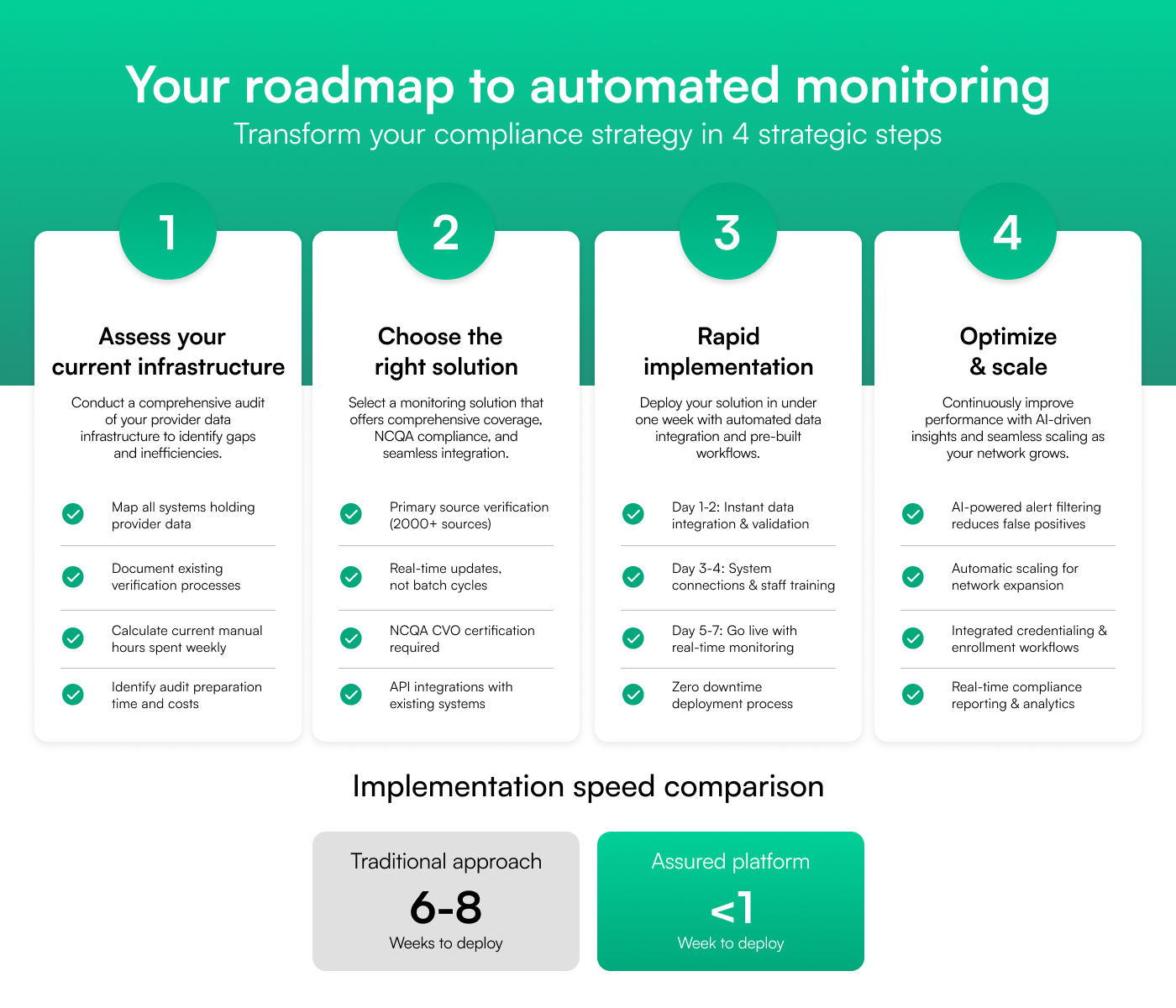
Here are four steps to follow:
Step 1: Assess Your Current Data Infrastructure
Before implementing any monitoring solution, conduct a comprehensive audit of your provider data infrastructure. Start by identifying every system that holds provider data—whether it's your credentialing software, HR platforms, spreadsheets, or shared drives.
Map out how data moves between these systems. Is information being synced automatically? Are manual transfers creating gaps or inconsistencies?
Document your existing verification process in detail, including:
- How license checks are performed
- Which sources are used for verification
- The frequency of updates
- How much work is done manually
Key questions to evaluate:
- How many hours does your team spend each week verifying credentials?
- How often do you discover expired licenses after the fact?
- What's your current audit preparation time?
- Are you relying on outdated databases or spreadsheets?
Understanding your baseline will help you quantify current inefficiencies and build a clear case for automation.
Step 2: Choose the Right Monitoring Solution
Once you understand your current gaps, the next step is to select a monitoring solution that fits your needs and scales with your organization. Not all credentialing software offers accurate monitoring. At a minimum, your solution should include:
- Primary Source Verification: It must connect directly to state medical boards, NPPES, DEA, OFAC, and other authoritative sources to ensure data accuracy
- Real-Time Updates: Look for a system that updates continuously, not in delayed batch cycles
- Comprehensive Coverage: The tool should monitor all 50 states and federal registries to eliminate blind spots
- NCQA Compliance: A CVO-certified platform ensures you’re always audit-ready
- Integration Capabilities: It should offer APIs or native integrations to connect with your current systems
To illustrate the difference between our tool and basic software, consider the following comparison:
As this demonstrates, fully automated platforms like Assured drastically reduce workload while increasing accuracy and audit preparedness. Choosing a solution should be based on the time saved, risk reduced, and compliance maintained.
Step 3: The Implementation Process
Most healthcare organizations assume that implementing credentialing software takes weeks, as it involves data migration, integrations, and staff training. Traditional implementations can last 4 to 6 weeks, delaying improvements and leaving compliance gaps open.
Thankfully, this doesn’t have to be the case as Assured takes a different approach by offering full deployment in under one week. Here’s how:
Day 1–2: Instant Data Integration
Assured automates the import of your current provider database, then validates every data point against 2,000+ primary sources. Gaps, expirations, and inconsistencies are flagged immediately.
Day 3–4: Seamless System Connection
Using pre-built integrations, Assured connects with your existing credentialing and HR systems in a matter of hours. It comes pre-configured with industry-standard workflows, eliminating the need to build from scratch. Staff can begin using the intuitive dashboard with minimal training. You can also customize alert settings based on your specific regulatory obligations.
Day 5–7: Go Live and Monitor in Real Time
By the end of the week, real-time license monitoring begins. You’ll get instant access to compliance reports and audit-ready documentation. Alerts are fine-tuned to match your organization’s risk tolerance and internal review process.
What makes this speed possible?
Assured comes equipped with pre-built integrations, automated data processing, healthcare-specific workflows, and a dedicated implementation team.
Step 4: Optimize Immediately
Unlike traditional platforms that require weeks of tuning, Assured begins optimizing from the start. The system continuously monitors its performance and automatically adjusts to ensure reliability and accuracy.
AI-driven alert filtering significantly reduces false positives, allowing your team to focus only on high-priority issues. As your provider network expands, the platform scales seamlessly to support new types of providers.
Credentialing and enrollment processes are also synced through integrated workflows. This ensures that once a license is verified or updated, the change is reflected across all connected systems instantly.
Compare the typical industry timeline to Assured’s:
With Assured, you get a fully operational, real-time compliance engine in less than seven days. Now that you know how to get real-time monitoring, how do you ensure that your tool’s verification will be across multiple data sources?
Keep reading to find out.
Ensuring Real-Time Verification from Multiple Sources
To effectively monitor healthcare providers, you need access to trusted, official databases. These sources help you confirm whether a provider is licensed, allowed to work, and free of any issues that could affect patient safety or your organization’s compliance.
These are the primary verification sources to have access to:
- State Medical Boards: License status, disciplinary actions, restrictions
- NPPES (National Provider Identifier): Provider demographics, practice locations
- DEA: Controlled substance registration status
- OFAC: Sanctions and exclusions screening
- SAM.gov: Federal contracting eligibility
- NPDB: Malpractice payments, adverse actions
However, just having access to these databases isn’t enough. You also need to check them at the correct times. Here are some verification best practices to look out for:
Verification Best Practices
Frequency Standards:
- License verification: Daily
- Sanctions screening: Real-time
- Board certification: Monthly
- Work history: At credentialing and re-credentialing
Data Quality Assurance:
- Cross-reference multiple sources for data accuracy
- Flag discrepancies for manual review
- Maintain audit trails for all verifications
- Regular system validation against known changes
Still, there are challenges. Every state has its own rules and processes for license verification, which makes it hard to follow a single workflow. Information from different sources often comes in various formats, so it has to be cleaned and standardized.
Some government databases update slowly or offer limited access through APIs, which can slow down your process. And then there’s the issue of false positives, as some systems can trigger too many unnecessary alerts.
That’s why a strong monitoring system needs to be smart, flexible, and built to handle these challenges, making sure your organization stays compliant without creating extra work.
Most importantly, your solution must be designed to automate compliance and audit readiness. We’ll explain how this happens in the next section.
Compliance and Audit Readiness Solutions
To stay compliant and audit-ready, healthcare organizations must meet the requirements of multiple oversight bodies, each with its standards. Here are a few:
- National Committee for Quality Assurance (NCQA) expects organizations to verify credentials directly from primary sources and to monitor licensing and sanctions on an ongoing basis. They also require detailed documentation of each verification, along with regular system audits and internal controls to catch gaps early.
- The Centers for Medicare & Medicaid Services (CMS) focuses on the accuracy of provider enrollment, providing timely updates when a provider’s status changes, and maintaining strict file integrity. These standards are especially critical for organizations that serve Medicare or Medicaid patients, as any compliance failure can lead to penalties or billing disruptions.
To stay ahead, many organizations now rely on automated solutions that generate audit-ready documentation in real time. How does this happen?
Automated Audit Preparation
Real-Time Documentation
Every verification is logged automatically with a timestamp. Each action includes a comprehensive audit trail that shows which source was checked, how it was checked, and the resulting outcome. Reports can be generated on demand. If something falls through the cracks, the system flags it with exception reporting so that no issue goes unnoticed.
Pre-Built Compliance Reports:
These platforms often come with pre-built reports that summarize key compliance data. For example, you can pull up a list of providers with upcoming license expirations, view a summary of sanctions screenings, or see a complete matrix of credential verification activities. These reports enable you to stay current with trends and demonstrate to regulators that your organization is adhering to best practices.
But how do you know that these systems are working to keep you audit-ready and compliant?
Here are some key performance indicators to track:
Compliance Metrics:
- Provider data accuracy rate (target: >98%)
- Average time to identify status changes (target: <24 hours)
- Audit preparation time reduction (benchmark: 80% improvement)
- Compliance violation incidents (target: zero)
Operational Metrics:
- Staff hours saved per month
- Cost per provider monitored
- System uptime and reliability
- User satisfaction scores
When it comes to return on investment, the numbers are precise.
Automating your monitoring and audit processes can save thousands of staff hours. For example, reducing 40 hours of manual work each week could save over $60,000 a year for an employee who earns the minimum hourly wage.
A single audit could cost $10,000 in preparation time alone. Additionally, automation reduces your technology costs by 60 to 80 percent compared to manual systems.
Beyond the numbers, failing to meet compliance standards has hidden costs. It can damage your reputation, disrupt your operations, delay provider onboarding, and even raise your insurance premiums.
By contrast, a well-designed compliance monitoring solution protects your entire organization. Despite the clear benefits of automating provider monitoring, many healthcare organizations hesitate when it comes to implementation. We’ll show you some of these obstacles and how to overcome them.
Overcoming Implementation Obstacles and Objections
Here are some of the common objections and how to deal with them:
1. IT Security Concerns: Many leaders are concerned about the risks of exposing sensitive provider data, particularly in light of the growing cybersecurity threats.
However, modern solutions like Assured are specifically designed for healthcare and meet the highest security standards. Assured is SOC 2 Type II compliant, utilizes end-to-end encryption, and features strict role-based access controls to ensure that only authorized personnel view the relevant data.
With over 1 million+ providers currently monitored, the platform has reported zero security incidents to date.
2. Legacy System Integration: Many organizations continue to use legacy software that provides limited or no API access, making it challenging to synchronize data automatically.
To solve this, Assured offers pre-built connectors for over 95% of the most commonly used healthcare systems.
For the few that aren’t supported out of the box, automated data import and export options provide a reliable backup, ensuring that no organization is left behind due to outdated tools.
3. Staff Resistance to Change: Staff members may worry that automation puts their jobs at risk, or they may simply feel overwhelmed at the idea of learning something new.
That’s why it’s important to present platforms like Assured not as a replacement, but as a way to make their jobs easier. The onboarding process typically takes just two to three hours, and ongoing support is always available to help staff feel confident and in control.
4. Budget Approval Challenges: It’s common for executives to question whether it is the right time to invest in new technology. But with compliance violations becoming more costly every year, the smarter move is to act early.
Assured is designed to deliver a return on investment within three to six months, primarily by reducing audit preparation time, cutting manual labor, and helping avoid costly penalties. For organizations that need proof first, a pilot program focused on a small group of providers can demonstrate the platform’s value without requiring a significant upfront commitment.
Why Organizations Delay Implementation (And Why They Shouldn't)
The cost of delay in automation is almost always higher than the cost of action. Still, many healthcare organizations delay implementation. Here are some misconceptions that sponsor this delay:
1. “We’re managing fine with current processes.”
On the surface, current systems may look like they’re working. Spreadsheets are filled out, deadlines are tracked manually, and audits are passed after a lot of hassle. But beneath the surface, there’s a sandhouse waiting to crash.
Little wonder 65% of organizations believe that leveraging automation will reduce the risk associated with compliance.
And the risks only grow. Annual compliance penalties increase by roughly 15% each year, staff are burnt out, and frustration is the order of the day.
2. “We’ll wait until the next budget cycle.”
Waiting for budget approval may seem like the best approach, but the hidden costs of delay add up fast. Every month, without automation leads to operational inefficiencies, like redundant credentialing tasks, payer rejections, and time spent managing spreadsheets.
Many compliance violations occur during these waiting periods, as no one is actively monitoring risk.
3. “We need more time to evaluate options.”
Evaluation is important, but when it drags on indefinitely, it becomes paralyzing.
Teams are stuck maintaining outdated tools while trying to assess new ones, and in the process, renewal dates are missed and audit readiness steadily declines.
Assured offers a way out of this. With under a week of implementation, there’s no need to commit six months to discovery before seeing value. You can get started, test it in your workflow, and integrate quickly without needing a long-term contract or massive IT investment.
4. “We’re not sure about the learning curve.”
Change is hard, but modern tools aren’t complex. Assured is designed to be intuitive enough for any team member to pick up with minimal instruction.
Most users are fully comfortable with the system in less than an hour. There’s no confusing backend interface. And during onboarding, your team is supported by a dedicated customer success manager who helps customize the platform to your needs and workflows.
If your staff can manage a credentialing spreadsheet, they can manage Assured. The barrier to entry is lower than it’s ever been.
Why Immediate Action Is Important:
- The regulatory pressure is increasing with the new NCQA standards practical from 2025
- Audit frequency is rising as CMS is expanding oversight across all organizational sizes
- Early adopters gain an operational efficiency edge
- Every day of delay increases compliance vulnerability
Now that you know why you should act quickly, your next question would be, “Would this work for the peculiarities of my organization and industry?” Let’s see some industry-specific use cases below.
Industry-Specific Use Cases and Applications
Different types of healthcare organizations face different compliance challenges, depending on their size, structure, and areas of service.
Assured is designed to adapt to each of these environments, offering targeted solutions that solve real operational problems at scale. Find out which use case is similar to yours:
1. For digital health companies, growth often happens fast and across state lines. A telehealth platform expanding from five to twenty-five states, for example, must navigate lots of state-specific licensing rules, DEA requirements, and credentialing processes.
What’s even worse? Traditionally, setting up these compliant operations in each state could take up to six months.
With Assured, the telehealth platform can simultaneously monitor licensing requirements across all 25 states. Automated tracking of multi-state licenses, renewal timelines, and regulatory changes enables digital health companies to scale faster, enter new markets quickly, and reduce compliance report processing time by up to 75%.
2. Large health systems and hospitals face a level of complexity that is unique: they must manage hundreds or even thousands of providers across various locations and specialties. In this environment, keeping provider records up to date and compliant is a massive task. Assured simplifies this by offering a centralized dashboard that tracks every provider in real time.
Whether you're credentialing physicians across multiple hospitals, managing short-term locum tenens arrangements, or overseeing a specialized surgical network, Assured keeps all records connected, accurate, and ready for audits. Academic medical centers can also utilize Assured to monitor the training of physicians and visiting faculty.
3. Hospital credentialing departments often face high volume and tight deadlines, processing dozens of new provider applications each month while still monitoring the credentials of their existing workforce. Assured automates primary source verifications and provides continuous license and sanctions monitoring, reducing credentialing time by 70% and helping teams maintain a 100% audit success rate, even as volume grows.
4. Telehealth and virtual care platforms face some of the most complex regulatory hurdles, from state-by-state telehealth laws to DEA registration requirements. Assured's telehealth-specific compliance tools help track these variations automatically, allowing companies to expand services across states without needing to scale their legal or compliance teams.
5. Multi-state provider groups, such as staffing agencies or traveling clinician networks, often struggle to stay on top of renewal deadlines across dozens of states. With Assured, they can consolidate all license information into one system and set up automated renewal alerts. This ensures operations run smoothly and renewals are on time, every time.
Let’s go on to explore the compliance regulations you’re up against in 2025 and beyond.
Regulatory Landscape and Compliance Requirements
Healthcare compliance is entering a new era, and the changes are raising the stakes for provider organizations of all sizes.
From January 2025, updated NCQA standards require more rigorous ongoing monitoring. At the same time, CMS is expanding its audit reach, especially targeting mid-sized organizations that were previously less scrutinized. Most state medical boards are moving from paper-based to fully digital license verification.
Telehealth regulations are also shifting, especially as more states join licensure compacts and introduce new compliance rules for virtual care providers.
There are also state-specific rules.
No two states handle licensing the same way. Some states, such as California, require providers to renew their licenses on an annual basis. Others, such as Texas, operate on a biennial cycle, and certain specialties follow a three-year renewal cycle.
States also differ in their continuing education rules, the reporting requirements for disciplinary actions, and the issuance or recognition of temporary licenses, such as those for locum tenens providers.
For multi-state organizations, keeping track of all this is a full-time job. With over 150 state medical and licensing boards, managing a single provider who practices in multiple states can mean juggling different timelines, rules, and systems. Sanctions and exclusions also vary by state, making real-time monitoring a necessity.
There’s more to these compliance changes.
Quarterly license and sanction verification is becoming the standard. Manual or paper-based tracking is being phased out, and regulatory bodies are moving toward a national credentialing database with unified standards. States are also doubling fines for non-compliance, and audit expectations are rising.
Organizations will need systems that can automate monitoring, issue real-time alerts, and create airtight audit trails. Compliance tools must also be able to integrate with evolving national and state databases to keep pace with these changes.
What are the penalties for failure?
License Compliance Failures:
- Expired License: $5,000-$50,000 per provider per violation
- Unreported Sanctions: $10,000-$100,000 depending on severity
- Inadequate Monitoring: $25,000-$250,000 for systematic failures
- Audit Documentation: $15,000-$75,000
Operational Consequences:
- Provider Suspension: Immediate revenue loss until compliance is restored
- Network Termination: Payer contract violations leading to removal
- Accreditation Risk: Joint Commission and NCQA sanctions
- Legal Liability: Malpractice exposure from non-credentialed providers
But can these systems integrate with your current workflow? And what tech specifications should you be working with?
Integration Capabilities and Technical Specifications
Assured is designed to integrate seamlessly into the healthcare technology stack, streamlining the compliance and credentialing processes.
Let’s see how the platform integrates into your stack and the technical specifications that make it your best bet.
EHR and Healthcare System Integrations
The platform offers pre-built integrations with leading EHR and healthcare systems, including Epic, Cerner (Oracle Health), Allscripts, athenahealth, and NextGen. These connections allow for deep, bidirectional data exchange.
API Documentation and Development
From a technical standpoint, the platform is developer-friendly and enterprise-ready. It provides a RESTful API with full support for create, read, update, and delete (CRUD) operations on provider records.
Developers can leverage webhooks to get real-time notifications when a provider’s status changes, and the system supports both JSON and XML data formats for flexible integration. Authentication protocols adhere to modern best practices, including OAuth 2.0 and API key management, while scalable rate limits ensure seamless performance, even for high-volume organizations.
Data Export/Import Capabilities
Provider data can be exported in multiple formats, including CSV, Excel, PDF, and custom templates, making it easy to generate reports or share information with external systems. On the import side, Assured supports bulk uploads, incremental updates, and real-time syncing from other databases.
Migration from legacy credentialing tools is supported through dedicated migration utilities and onboarding support.
Workflow Automation Examples
Credentialing teams can automate tasks such as license renewal alerts at 90-, 60-, and 30-day intervals, as well as provide real-time updates to credentialing statuses and automatically generate reports for audits.
Security and Compliance Features
All of this is backed by enterprise-grade security: AES-256 encryption, strict role-based access controls, full audit trails, and certifications for HIPAA, HITECH, and SOC 2 Type II.
Ultimately, these high-level technical specifications would make your automation workflow a breeze. But if you plan to stick with your manual systems, what are the odds that they will fail? And what risks do you stand to face, should they fail?
Failure Scenarios and Risk Mitigation
When credentialing and compliance systems fail, the consequences are immediate and costly.
During audits, even a 15% rate of expired provider licenses can result in significant penalties.
The financial impact might reach $500,000, with an additional $200,000 spent on remediation efforts, not to mention the reputational damage. Restoring full compliance could take anywhere from three to six months.
Real-world examples make the risks tangible. A missed license expiration might allow a provider to continue practicing illegally, putting patients and the organization at risk. An unreported sanction could trigger an Office of Inspector General (OIG) exclusion notice, which may be discovered only during a payer audit. Systems that don’t actively monitor provider credentials can leave compliance gaps unnoticed, while incomplete verification records make it impossible to defend against audit findings.
Revenue and Operational Impact
Beyond fines, compliance failures can have a significant impact on operations. If a provider is suspended, patients must be reassigned, appointments are canceled or delayed, and the quality of care suffers.
Financially, organizations may lose $10,000 to $50,000 per suspended provider per month. Additional payer audits can delay reimbursements, and legal exposure grows if non-credentialed providers deliver care. Even insurance premiums may rise due to increased risk.
Assured's Risk Prevention
Assured reduces these risks through proactive monitoring and failure recovery:
Proactive Monitoring:
- Continuous Verification: Real-time status updates prevent lapses
- Predictive Alerts: Advanced notice of potential compliance issues
- Automated Documentation: Complete audit trail for every verification
- Redundant Systems: Multiple verification sources ensure accuracy
Failure Recovery:
- Immediate Notifications: Instant alerts for any compliance changes
- Rapid Response: 24/7 monitoring ensures quick issue resolution
- Expert Support: Dedicated compliance team for complex situations
- Audit Assistance: Complete documentation support during reviews
But does Assured cover multiple geographic locations? Let’s find out.
Geographic Coverage and Multi-State Licensing
Credentialing across multiple states can be complex, but Assured offers comprehensive coverage and seamless tracking across all 50 states, U.S. territories, and relevant federal databases. Here’s how:
- Real-time integration with every state medical board ensures that licensure data is always up to date.
- Assured supports all major interstate compacts. The Nurse Licensure Compact, Interstate Medical Licensure Compact, Psychology Interjurisdictional Compact (PSYPACT), and EMS Compact are tracked automatically, allowing credentialing teams to monitor eligibility and status changes as providers move or expand their scope.
- Centralized dashboard: Organizations dealing with border-state licensing, locum tenens staffing, or rapidly growing telehealth operations often struggle with renewal timing, unique documentation rules, and reporting inconsistencies. Assured simplifies this with a centralized dashboard that shows all active licenses, sends alerts for renewals based on each state’s rules, and reduces costs through consolidated license management.
- International credentialing: Assured verifies foreign medical degrees through ECFMG and other accepted sources, tracks international license validity, and monitors visa status for providers on H-1B or similar programs.
Now that we’ve shown you how automated real-time monitoring helps you fix provider data compliance issues, the next step is choosing the right solution provider for you.
Choosing the Right Solution Provider
Now that we’ve shown you how automated real-time monitoring helps you fix provider data compliance issues, the next step is choosing the right solution provider for you.
When evaluating a provider monitoring solution, it’s essential to look beyond surface-level features. Here are some factors to consider:
- Technical Capabilities: The right platform should be technically strong, easy to integrate, and designed with healthcare in mind. Start by making sure the solution is NCQA Certified as a Credentials Verification Organization. Look for integrations with primary sources, along with real-time alerts and API support, to seamlessly plug into your existing systems.
- Industry Experience: Experience in healthcare is just as necessary as the tech itself. You want a partner that understands healthcare regulations and has a track record of success with organizations like yours. References, case studies, and measurable outcomes can offer clarity on what to expect.
The Assured platform stands out as the premier choice for monitoring healthcare provider data.
Key Differentiators:
- NCQA Certified CVO: Meets highest industry standards
- 2000+ Verification Sources: Most comprehensive coverage available
- 80% Time Reduction: Proven efficiency improvements
- Real-Time Monitoring: Instant status updates and alerts
- 95% Accuracy Rate: Industry-leading precision
Assured’s automation eliminates the need for manual monitoring, freeing up hours of administrative time every week. Teams gain access to a centralized dashboard that organizes provider records, automates verification, and sends customized alerts as needed.
Built-in reporting tools make the audits easy, and seamless integration with major EHRs ensures smooth workflows. For organizations looking to reduce costs, boost accuracy, and maintain full compliance, Assured consistently delivers, with a 100% audit success rate and 50–60 hours saved per week.
Implementation Success Factors
The successful implementation of an automated provider monitoring system depends on several key factors.
- Leadership Support: When executives support the project, it becomes easier to secure the necessary resources and gain staff buy-in.
- Change Management: This involves communicating what’s changing, why it matters, and providing training so that staff feel confident using the new system.
- Data Quality: Clean, accurate data from the start sets the tone for reliable monitoring.
- Integration Planning: This helps the new tool blend into existing workflows without disruption.
There are also common missteps to watch out for. Many teams underestimate the time required to clean up provider data before launch. Without enough training, users may resist the change or make mistakes. Additionally, if alerts are poorly configured, they can overwhelm staff with excessive and unnecessary notifications. And if the system isn’t properly tested before going live, even minor glitches can slow down adoption.
Measuring Implementation Success
30-day success metrics:
- System uptime and performance stability
- User adoption rates across departments
- Data accuracy improvements over baseline
- Initial time savings and efficiency gains
90-day success metrics:
- Full workflow integration completion
- Compliance metrics improvement
- ROI achievement and cost savings realization
- Staff satisfaction scores and system feedback
If you’ve read this comprehensive guide on using automated real-time monitoring, it’s time to get started. Now, let’s wrap things up.
Transform Your Compliance Strategy Today
Finally, healthcare provider data compliance no longer needs to be a stressful, resource-draining task.
With automated, real-time monitoring, compliance becomes less reactive and more strategic or proactive. Organizations using these tools reduce compliance risks by up to 95%, save 40 to 60 hours a week in manual effort, and reach full audit readiness with NCQA-certified solutions. Most see a measurable return on investment within three to six months.
At this point, the real question isn’t whether to implement automated monitoring. It’s how soon you can get started.
The technology is ready and the results are proven. The only thing left is to act.
If you’re ready to take control of compliance, start by auditing your current processes, calculating the actual cost of manual verification, and exploring NCQA-certified solutions, such as Assured, that meet your needs.
Ready to eliminate provider data compliance issues? Book a demo to see how Assured can help you stay ahead.



.png)


.png)


