Credentialing and payer enrollment are often used interchangeably, but they’re not the same thing. While they both play a role in bringing a new provider on board, they handle two very different parts of the process.
Credentialing verifies a provider’s qualifications, and payer enrollment ensures they can get reimbursed for their services. If either one is delayed, revenue stalls, providers sit idle, and patients wait longer for appointments. These delays can cost hospitals more than $7,500 per day, per physician in lost revenue.
In this guide, we’ll break down how credentialing and payer enrollment work, where they differ, and how to manage both more efficiently to avoid unnecessary delays and revenue loss.
What provider credentialing actually verifies (And why it takes 90–150 days)
Credentialing is the foundation of provider onboarding. It’s the process that confirms whether a provider is qualified, not just on paper, but in a way that meets your organisation’s internal policies, payer requirements, and regulatory standards. Without credentialing, providers can’t treat patients, and you can’t submit claims.
What gets verified during credentialing
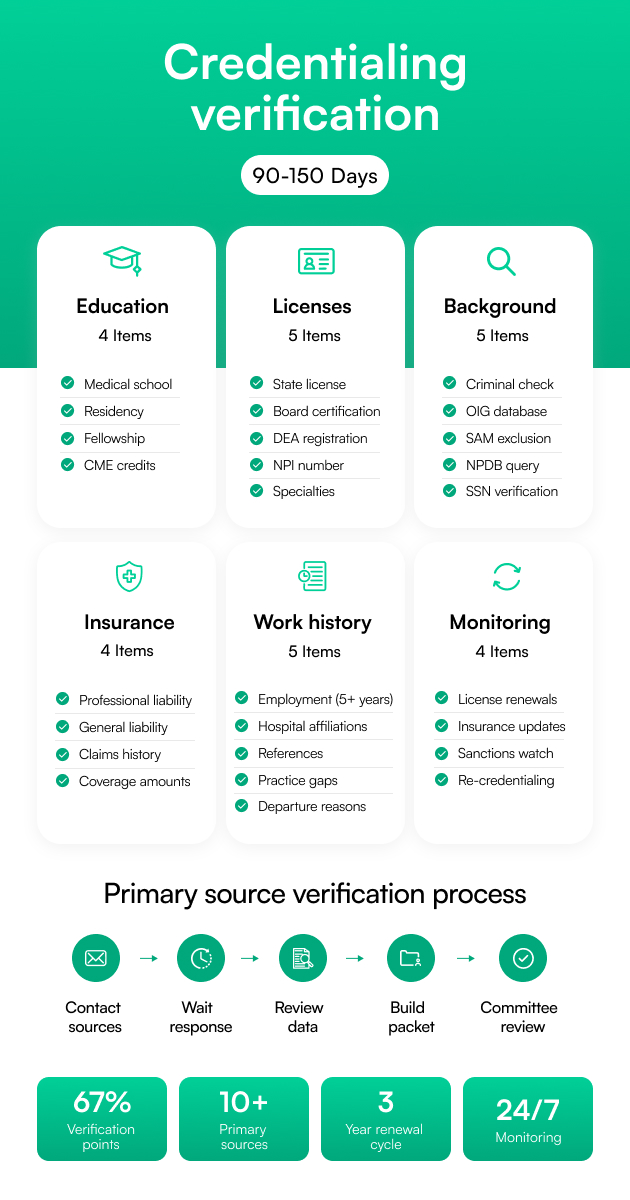
Credentialing includes:
- Medical education and training: Verification of medical school, residency, and fellowship completion.
- Board certifications and state licenses: Confirming active and unrestricted certifications and licensure.
- DEA registration and malpractice insurance: Ensuring proper authority to prescribe and required liability coverage.
- Work history, references, and background checks: Looking for gaps, red flags, or inconsistencies.
Each item needs to be cross-checked with primary sources (like state boards, medical schools, or the DEA), which can take time, especially when done manually.
4 types of credentialing every organization needs
Depending on your organization’s structure and provider network, you may need to manage one or more of the following:
1. Initial Credentialing
This is the most intensive phase, verifying a provider’s qualifications for the first time. It typically takes 90 to 150 days, depending on provider responsiveness, document completeness, and verification turnaround times.
2. Recredentialing
A provider isn’t credentialed for life. Recredentialing is typically required every 3 years to confirm that licenses, certifications, and work history remain up to date.
3. Delegated credentialing
In some cases, payers allow your organization to perform credentialing on their behalf. It speeds up enrollment but requires strict adherence to NCQA or URAC standards.
4. Multi-state credentialing
Especially relevant for telehealth or multi-location practices, this involves verifying licensing and compliance across multiple states, and adds complexity to an already detailed process.
Typical costs: $3,000–$5,000 per provider
Depending on your team's structure, the cost per provider (including labor, delays, and third-party services) can range from $3,000 to $5,000 or more.
So, what drives those costs?
Well, timeline factors and common delays such as missing documentation, provider inaction, slow responses from primary sources, and manual data entry.
Who performs credentialing?
The credentialing process may be the same in principle, but who handles it can make all the difference in speed, accuracy, and cost.
Let’s look at the three main models:
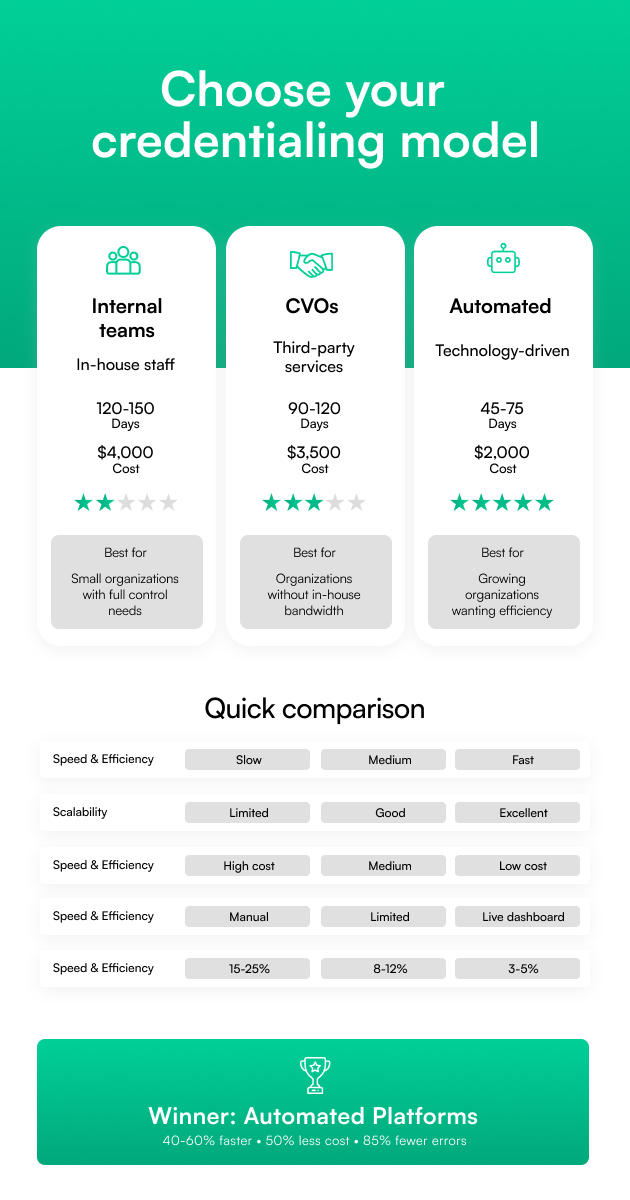
1. Internal credentialing teams
Many hospitals, health systems, and mid-sized practices rely on in-house credentialing coordinators or medical staff services departments. These teams are often responsible for gathering documentation, contacting primary sources, and keeping everything organized, usually across multiple spreadsheets, emails, and filing systems.
Pros:
- Full control over the process
- Easier to align with internal policies and preferences
- Often more responsive to provider needs
Cons:
- Labor-intensive and time-consuming
- Hard to scale, especially during high-growth periods
- Higher risk of human error and missed deadlines
Internal teams work best when volume is low to moderate, or when combined with technology that automates some of the most repetitive tasks.
2. Centralized verification organizations (CVOs)
A CVO is a third-party service that handles credentialing on your behalf. They contact primary sources, compile provider packets, and ensure all verifications meet compliance standards, typically those set by NCQA, URAC, or The Joint Commission.
Pros:
- Takes the burden off your internal team
- Typically compliant with industry standards
- Helpful for smaller teams or those with high credentialing volume
Cons:
- Less flexibility in workflow and turnaround
- May require handoff delays or duplicate data entry
- Still reliant on manual effort and email follow-ups
CVOs are a popular choice for organizations that don’t have the bandwidth or staff to manage credentialing in-house.
3. Automated credentialing platforms
Modern credentialing platforms, like Assured, combine automation, tracking, and real-time data integrations to handle credentialing faster and with far fewer errors. These platforms streamline primary source verifications, manage expirables, track progress, and integrate with CAQH, PECOS, and state licensing boards.
Pros:
- Cuts credentialing time by 40–60%
- Reduces human error and duplicate data entry
- Centralizes documents, deadlines, and communication
- Scales easily with growing provider networks
Cons:
- May require internal training or process adjustment
- Some legacy systems might resist integration
If you're still relying on manual processes or legacy CVOs, transitioning to an automated platform can drastically speed up onboarding and reduce overhead.
What payer enrollment actually does (And why you can't bill without it)
Before a provider can see patients and submit claims, they need to be officially enrolled with the insurance companies you work with. Payer enrollment establishes the billing relationships that allow your organization to get reimbursed for services.
What is payer enrollment?
Payer enrollment is about registering a provider with public and private insurance companies. It’s how you get listed in a payer’s system, negotiate reimbursement rates, and obtain the credentials needed to start billing.
It’s a required step for every provider who expects to be paid by Medicare, Medicaid, or commercial insurers.
What Happens During Payer Enrollment
The process involves multiple parts:
- Submitting applications through government portals like PECOS (for Medicare), individual state systems (for Medicaid), or third-party systems like Availity (for commercial plans).
- Negotiating contracts and fee schedules with payers, depending on your organization’s structure.
- Obtaining billing IDs and credentials that allow you to submit claims and receive payment.
- Updating CAQH profiles, collecting required documents (like W-9s and board certifications), and tracking submission statuses.
Timeline Reality: 60–180 Days Per payer
The truth is that payer enrollment is rarely quick, and delays are common, especially if applications are incomplete, credentialing isn’t finished, or documentation is outdated.
Here’s what to expect:
- Medicare (PECOS): 60–90 days, assuming all documentation is in order
- Commercial payers: 90–120 days on average, though some are faster with delegated arrangements
- Medicaid: Timelines vary widely by state, but typically range between 60 and 180 days
Because each application runs independently, even one missing signature can delay the entire process, putting both patient access and revenue at risk.
What’s the Difference Between Payer Enrollment and Provider Credentialing?
Provider onboarding steps (Credentialing + Enrollment)
Here’s what a typical end-to-end onboarding flow looks like:
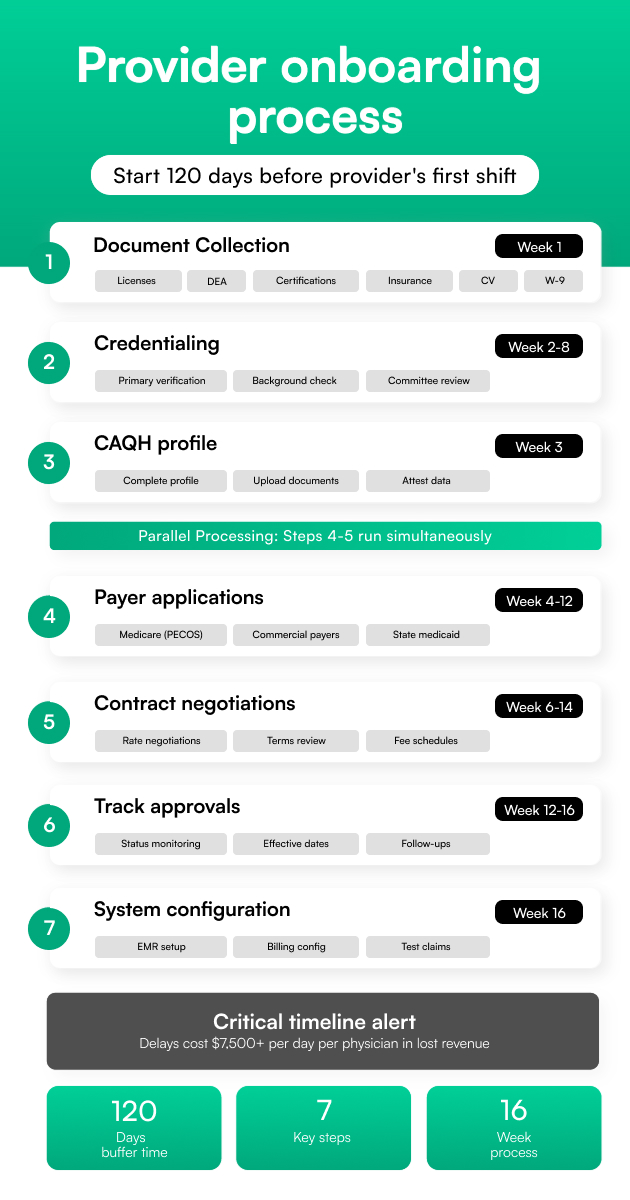
- Collect All Required Documents Early
Start by gathering licenses, DEA, board certifications, malpractice insurance, CVs, W-9s, and any state-specific forms. Missing just one document can stall the entire process
- Complete Credentialing
Run primary source verifications (PSV) and ensure all training, licensure, and work history are validated. This forms the foundation of trust and compliance
- Build or Update the CAQH Profile
Make sure the provider’s CAQH profile is complete, current, and attested; most commercial payers will pull data directly from here
- Submit payer Applications
Use portals like PECOS (for Medicare) or payer-specific platforms. Include all required attachments and signatures
- Handle Contract and Fee Negotiations
This is where reimbursement rates, participation terms, and group agreements get finalized. It’s important not to rush through this part
- Track Approvals and Effective Dates
Keep an eye on enrollment status and go-live dates. Delays here can cause claim denials or missed billing windows
- Configure EMR and Billing Systems
Once approvals come in, ensure provider info is entered correctly into your EMR, billing software, and clearinghouse systems to avoid downstream issues
Pro Tip: Start the onboarding process at least 120 days before a provider’s first scheduled shift. That gives you enough buffer time for credentialing delays.
Navigating the credentialing and enrollment process
Although credentialing and payer enrollment are two separate workflows, they’re deeply connected, and successfully navigating both depends on understanding the tools, systems, and timelines involved.
CAQH: Your provider data home base
CAQH (Council for Affordable Quality Healthcare) is a nonprofit alliance of health plans and industry stakeholders. They are well-known for their CAQH ProView platform.
The CAQH ProView is a centralized online database where healthcare providers store their professional information, licenses, education, work history, malpractice insurance, certifications, and more. This data is then shared with insurance companies and hospitals for credentialing and payer enrollment.
Providers (or their admins) must regularly update and attest to the profile on CAQH, especially before submitting enrollment applications. A lapse here can easily delay or derail enrollment altogether.
PECOS: Medicare-specific enrollment
For Medicare enrollment, PECOS (Provider Enrollment, Chain, and Ownership System) is the platform you’ll use.
It requires its logins, approvals, and documentation flow, separate from CAQH. Timelines vary, but it often takes 60 to 90 days from submission to approval. If your Medicare PECOS application is incomplete or if it doesn’t match your credentialing data, it can trigger further delays.
Payer-specific quirks
Each commercial payer has its own rules, timelines, and systems:
- Some accept delegated credentialing if your organization is approved.
- Others require complete, manual enrollment with custom documentation.
- Some use third-party portals, while others stick to proprietary systems.
- Effective dates aren’t always precise, and approvals can be silent; you have to keep checking.
Due to these quirks, a centralized platform for managing all payer workflows is a more effective solution.
Tracking timelines and status per payer
Every payer moves at a different pace. Some might approve within 45 days, while others take over 120. Without a clear system for tracking application status, documents submitted, and next steps, it’s easy to lose visibility.
This is where automation and centralized dashboards make a big difference; they give you a real-time view of where every provider stands with every payer, so you’re never left guessing.
Payer enrollment application process (Step-by-Step)
Enrolling a provider with one or multiple insurance payers can be a long, detail-heavy process, but when you break it down step-by-step, it becomes much more manageable.
Here’s how to move through the payer enrollment process efficiently, while reducing the risk of delays or rejections:
1. Confirm credentialing completion
Before enrolling a provider with any payer, ensure their credentialing is either complete or nearly finalized. Most payers require verified credentials before they'll even review an enrollment application. Ideally, start enrollment when credentialing is about 80% complete so the two timelines run in parallel without challenges.
2. Complete CAQH profile and attest
Most commercial payers (and even some Medicaid plans) use CAQH to verify provider data. Ensure the provider’s CAQH profile is filled out accurately, and don’t forget to attest to the information; this signals to payers that the data is up to date.
3. Gather payer-specific documents
Each payer may ask for slightly different documentation. Typical requirements include the provider’s state license(s), DEA registration, malpractice insurance, CV, board certifications, and a signed W-9. Creating a checklist for each payer helps keep the process organized and audit-ready.
4. Submit applications via PECOS, availity, or direct Portal
Use PECOS for Medicare applications. Submit directly through the payer's online portal when required.
Make sure all forms are filled out entirely and uploaded in the correct format. Any missing fields can cause the application to be kicked back.
5. Monitor application status
Once submitted, don’t assume things are moving; check on the status regularly. Many payers don’t proactively notify you of missing information. A good enrollment platform will offer real-time status tracking and reminders for follow-ups.
6. Obtain payer IDs and billing credentials
Once approved, you’ll receive confirmation in the form of a payer ID, welcome letter, or billing credential packet. These are essential for activating the provider in your billing system and submitting clean claims.
7. Validate billing readiness
Before the provider sees their first patient, make sure their billing profile is live in your EMR or practice management system. Double-check that the payer IDs are entered correctly, contracts are loaded with the right fee schedules, and all effective dates are in place.
How to integrate enrollment and credentialing
The most efficient organizations treat enrollment and credentialing as two parts of the same provider onboarding journey, connected by shared data, intelligent workflows, and timing.
Here’s how to bring them together:
1. Use a shared provider profile (Let CAQH be your source of truth)
Instead of duplicating provider data across multiple systems, anchor everything to a single, centralized profile, usually the provider’s CAQH record. Credentialing teams can verify qualifications, and enrollment teams can pull directly from that same profile for payer submissions. It keeps everyone aligned and eliminates version control issues.
2. Let credentialing drive the enrollment timeline
Enrollment shouldn’t start too early, but it also shouldn’t wait until credentialing is fully done. Begin preparing enrollment once credentialing is about 70–80% complete. This gives you time to collect payer-specific documents, update CAQH, and queue up submissions so there’s no lag when credentialing wraps.
3. Automate the hand-off with alerts and workflows
The best systems use built-in workflows to trigger tasks automatically. For example, once a provider’s license and board certifications are verified, your system should alert the enrollment team to begin their steps.
4. Eliminate redundancies
If your credentialing and enrollment teams are entering the same provider data into different tools, you're wasting time and increasing the risk of errors. A unified system, or at the very least, integrated tools, will help you avoid double entry, reduce confusion, and speed up onboarding.
Automation tools that actually save 40+ hours per provider
The right automation tools can completely transform the process—saving your team time, cutting down on costs, and getting providers onboarded weeks faster.
Here’s what to look for in a credentialing and payer enrollment platform.
- Auto-Verification
Look for direct integrations with medical boards, DEA, NPI Registry, and other primary sources. This eliminates the need for back-and-forth emails, drastically speeding up verification timelines.
- CAQH Integration
The platform should automatically sync provider data with CAQH and send reminders to attest every 120 days. This alone can eliminate one of the most common challenges in commercial payer enrollment.
- Bulk Submissions
Instead of filling out separate applications for every payer, choose a platform that lets you submit to multiple payers at once, using innovative templates and auto-fill features to avoid rework.
- Renewal Tracking
Licenses, contracts, DEA registrations, malpractice insurance, everything has an expiration date. An automated system should send alerts ahead of time and even kick off the renewal process for you.
ROI numbers that matter
When automation is done right, the return shows up in real-world gains you can measure:
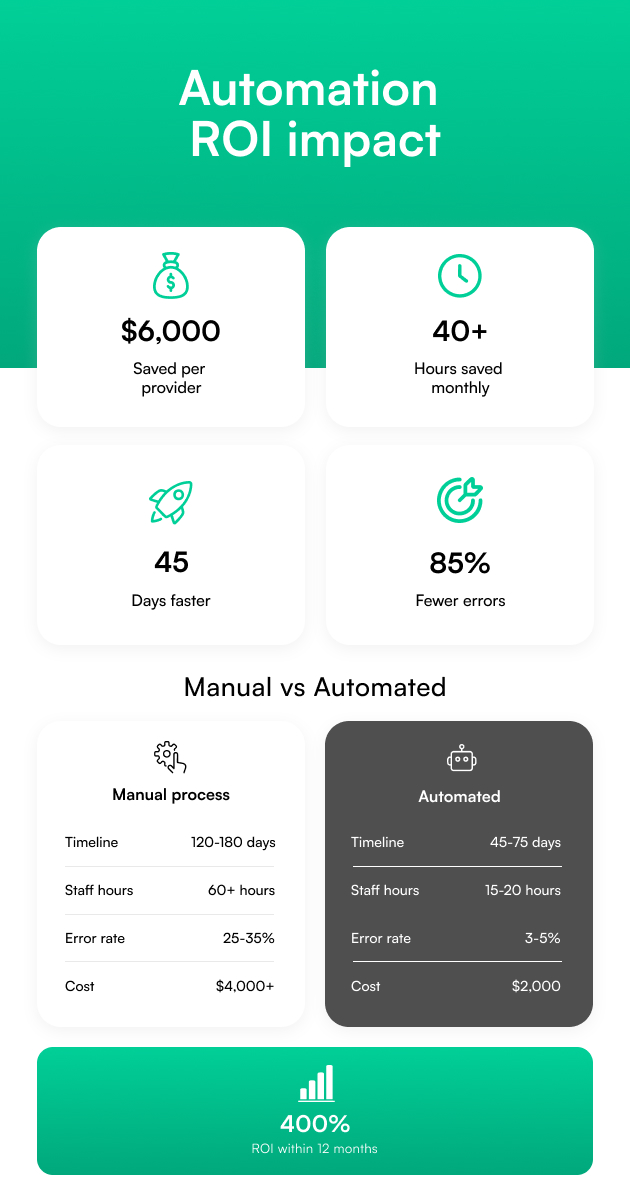
- Time Savings: Save 40+ hours per provider per month by eliminating manual entry and chasing paperwork
- Speed Improvement: Cut onboarding timelines by 30–50%, helping providers start seeing patients faster
- Cost Reduction: Save $60K+ annually for every 10-provider team by reducing admin overhead and denied claims
- Error Reduction: Up to 85% fewer rejections due to incomplete or inaccurate applications
How platforms like Assured deliver these results
Assured was built to streamline and simplify the most painful parts of credentialing and enrollment, without sacrificing compliance or control. Here’s how the platform works:
- Primary Source Verification Automation
Instantly verify education, licenses, and certifications using real-time source integrations.
- One Unified Dashboard
See the complete status of every credentialing and enrollment task, across all payers, providers, and states, in one place.
- Hands-On Support for Complex Cases
Get expert help navigating delegated credentialing, multi-state licensing, or high-volume payer enrollments.
- Built-In Compliance Tools
Stay audit-ready with real-time tracking, automated alerts, and reports aligned with NCQA and CMS standards.
The right automation isn’t just about doing things faster, but about getting providers working, revenue flowing, and teams breathing a little easier. That’s the kind of impact platforms like Assured are designed to make.
Best practices for automated credentialing and enrollment
Even with automation, success depends on building solid workflows and maintaining accurate data. Here are a few proven best practices that make a real difference:
1. Centralize provider data
Keep all provider records, documents, verifications, notes, and updates in one centralized system. This eliminates version control issues, prevents data silos, and makes it easier to share information across credentialing, enrollment, HR, and compliance teams.
2. Standardize document intake
Establish a standardized checklist for collecting essential documents from each provider, including W-9 forms, licenses, malpractice certificates, references, DEA and CSR registrations, and board certifications. Standardization avoids last-minute scrambles and makes your onboarding process faster and more predictable.
3. Monitor expiration dates proactively
An automated system should track timelines and send alerts well in advance. Letting even one of these lapse can not only trigger compliance issues but also lead to denied claims and unnecessary revenue loss.
4. Track payer effective dates and revalidations
Once a provider is enrolled, your work isn’t over. Keep a close eye on effective dates (when reimbursement begins) and payer-specific revalidation schedules. Missing these windows can disrupt billing and require the provider to go through the whole enrollment process again.
5. Use software with payer-specific workflow templates
Not all payers ask for the same things, in the same way, at the same time. Using software that includes payer-specific workflows helps you submit the proper forms, avoid back-and-forth, and reduce denials. These prebuilt templates make it easier for you to navigate multiple portals, formats, and requirements.
Benefits of streamlining both processes
By aligning both credentialing and payer enrollment, healthcare organizations can start witnessing serious, impactful results such as:
1. Faster onboarding
When credentialing and enrollment run on parallel, automated tracks, providers can start seeing patients sooner. Instead of waiting months to get cleared and contracted, they’re up and running in weeks, not quarters.
2. Fewer claim denials
Delays or mismatches between credentialing and enrollment data are a top reason claims get rejected. A unified system reduces errors, ensures payer requirements are met up front, and prevents costly back-and-forth corrections later.
3. Shorter time to revenue
The longer it takes to get a provider enrolled and approved by payers, the longer it takes to collect payment. Streamlining both processes means fewer revenue gaps from delayed start dates or rejected submissions.
4. Stronger provider satisfaction
Providers want to do what they were hired to do: care for patients. If onboarding drags on for months, it creates frustration and damages trust. A smoother process shows providers that your organization is well-run and values their time.
5. Cleaner audits and documentation trail
Regulatory audits are much easier to navigate when your credentialing and enrollment data is centralized, consistent, and well-documented. With a clean digital trail, you can demonstrate compliance and respond to requests quickly, without scrambling for paper files or chasing missing information.
Risks of mismanagement
When the process of provider enrollment is slow or mismanaged, the ripple effects can be costly and difficult to recover from.
Here’s what’s at stake if enrollment isn’t handled correctly:
1. Delayed payments = major revenue loss
Every month a provider isn’t enrolled, your organization could be losing $30,000 to $100,000 or more in unbillable services. Multiply that across multiple new hires, and the financial impact adds up fast.
2. Out-of-network billing = denied claims
If a provider isn’t officially enrolled but still delivers care, you’re forced to bill out-of-network. That usually means rejected claims, lower reimbursement rates, and lots of extra back-and-forth with the payer, all of which slow down cash flow.
3. Billing before enrollment = false claims risk
Submitting claims before a provider is fully enrolled puts your organization at risk for false claims violations. This is a serious compliance issue that can trigger audits, penalties, and legal trouble.
4. Slow onboarding = provider frustration and churn
When providers have to wait weeks (or months) before they can treat patients and get paid, frustration builds. Delays in ramp-up time can hurt morale, increase turnover, and make it harder to recruit in the future.
5. Compliance gaps = CMS or NCQA trouble
Inconsistent or poorly documented enrollment processes can put your organization out of alignment with CMS, NCQA, or Joint Commission guidelines. That means exposure during audits, or worse, a loss of accreditation.
Challenges in credentialing and enrollment
Credentialing and payer enrollment are both essential, but they’re also notoriously difficult to keep running smoothly. Here are some of the most common challenges healthcare organizations face:
1. Payer delays and backlogs
Most payers, especially government programs like Medicare and Medicaid, operate with limited staffing and high application volumes. As a result, even well-prepared submissions can sit in a backlog for weeks or months. Without proactive follow-up, applications often get stuck in limbo with no clear timeline for approval.
2. Missing or inconsistent provider data
Credentialing and enrollment rely on having clean, complete, and consistent provider information across licenses, education history, work experience, and personal details. One typo or mismatch between systems can lead to rejected applications or unnecessary rework.
3. Lack of CAQH attestation
Even if a provider’s CAQH profile is filled out correctly, it won’t be considered “active” unless they’ve attested to the information within the past 120 days. Missed attestations are one of the top reasons commercial payers reject or delay enrollment.
4. Managing renewals across multiple systems
Keeping track of expiring state licenses, DEA registrations, and recredentialing timelines across multiple systems can quickly overwhelm internal teams, especially without a centralized dashboard or automated reminders.
5. State-by-state medicaid requirements
Medicaid enrollment is particularly tricky because every state has its own rules, portals, timelines, and required documentation. A strategy that works in California might not apply in Texas, Georgia, or New York. Navigating these differences manually can significantly slow down provider onboarding.
Expected ROI: What organizations actually save
When organizations switch from manual processes to automated platforms, they save money and time, accelerate revenue growth, and build a more scalable operation that grows without burning out their teams.
Year 1 financial returns
- Cost Savings: Most organizations see savings of $5,000 to $7,000 per provider in their first year just by eliminating manual work, follow-ups, and rework tied to credentialing and enrollment.
- Revenue Acceleration: With automation in place, providers are enrolled and billing-ready 45 days faster, meaning claims go out sooner, and payments come in quicker.
- Staff Efficiency: Automation reduces administrative workload by 50–60%, freeing up your team to focus on higher-value work (instead of chasing down documents or logging into half a dozen portals).
- Overall ROI: Many organizations report a 300–400% return on their credentialing and enrollment platform investment, often within the first 12 months.
Long-term strategic benefits
- Scalability: Add new providers or expand into new states without hiring more credentialing staff; the system does the heavy lifting.
- Competitive Advantage: Beat other organizations with faster onboarding, making your offers more attractive to top-tier providers.
- Compliance Confidence: With built-in alerts and real-time monitoring, you stay audit-ready and avoid costly oversights that come with manual tracking.
- Provider Satisfaction: A smoother onboarding experience (with fewer delays or resubmissions) leads to a 60% improvement in provider satisfaction, which means better retention and stronger team morale.
Conclusion: Credentialing and enrollment from one platform
Credentialing ensures your providers are qualified to deliver care. Payer enrollment ensures they get paid for it.
You can’t have one without the other. If either process is delayed or incomplete, it slows everything (patient access, cash flow, and your ability to grow).
That’s why the most efficient healthcare organizations are moving toward platforms that bring both workflows under one roof.
Tools like Assured help you manage credentialing and enrollment with automation, real-time tracking, CAQH integration, and audit-ready documentation.
If you’re ready to simplify provider onboarding, book a demo with Assured to get started.
FAQs
1. Can I bill before I’m fully enrolled?
Generally, no, unless using locum tenens or under a supervising provider’s NPI.
2. Do I need both processes for telehealth providers?
Yes. You still need credentialing and payer enrollment, even across state lines.
3. How often do I need to retest in CAQH?
Every 120 days.
4. Is delegated credentialing faster?
Often yes, but only if the payer allows it.


.png)


.png)