For Chief Medical Officers (CMOs), credentialing isn’t just an administrative task; it’s an important part of protecting patients, ensuring timely access to care, and upholding the integrity of the entire organization.
When credentialing is delayed, the consequences go far beyond lost time. Patient safety is compromised, clinical outcomes are affected, and organizations face real financial and regulatory exposure.
Take this common scenario: a CMO is alerted to a near-miss incident—a provider with an expired license, overlooked due to a credentialing backlog, was scheduled to perform a high-risk procedure. The issue was caught just in time, but the outcome could have been catastrophic. Beyond the clinical risk, the financial penalty for such an oversight can range from $100 to $50,000 per HIPAA violation, with a maximum of $1.5 million yearly. And that doesn't begin to capture the reputational damage.
When these lapses go unnoticed, the impact multiplies: delayed care, breakdowns in compliance, and lost revenue, often exceeding $14,000 a day for each affected specialist.
So, how can CMOs take control? It starts with streamlining the credentialing process through modern, technology-driven solutions. Platforms like Assured reduce credentialing timelines from 60–90 days to just 2 days (48 hours). By doing this, they improve safety, accelerate access to care, and save up to $1.5–$2 million annually across a 300-provider network.
As a CMO, it’s time to put safety and speed first. Book your free Assured consultation today.
Why Credentialing Impacts Patient Safety: CMO Challenges
Credentialing is a frontline defence against unsafe care. However, outdated systems and manual processes threaten that safety net.
Here’s how credentialing can impact patient safety.
1. Care Gaps from Delays
Most credentialing processes take 60–90 days. During that time, a qualified physician may be idle while patients wait. This is especially dangerous in high-acuity specialties like oncology or surgery. A newly hired oncologist delayed by two months can mean dozens of cancer patients waiting weeks for diagnosis or treatment. It's not just inefficient, it's also unsafe.
2. Unverified Providers
In most hospitals, credentialing still relies on spreadsheets, email chains, and overworked staff manually tracking license renewals.
These manual credentialing processes make it easy for providers to miss expiration dates for licenses, board certifications, or insurance coverage. When this happens, providers unknowingly deliver care while unqualified, putting patients and your organization at serious risk.
3. Regulatory Exposure
CMS (Centers for Medicare and Medicaid Services) and The Joint Commission have strict rules regarding credentialing and privileging. Credentialing delays or errors can result in fines ranging from $100 to $50,000 per violation.
But for most CMOs, the bigger concern is the reputational hit from a published safety lapse. One publicized failure can undermine years of patient trust.
4. Operational Strain
Credentialing staff often manage thousands of data points across hundreds of providers. According to industry estimates, overworked teams managing 1,500+ data points manually increase error rates by 15%.
These errors can lead to bigger risks, like credentialing gaps, expired documents, or missed alerts that directly impact patient safety.
Assured is built to eliminate these risks.
Assured: Your Partner in Patient Safety Through Credentialing
More than just a credentialing software, Assured is a safety engine, created to verify providers quickly, keep your system compliant, and reduce patient risk.
Here’s how Assured steps in to help CMOs:
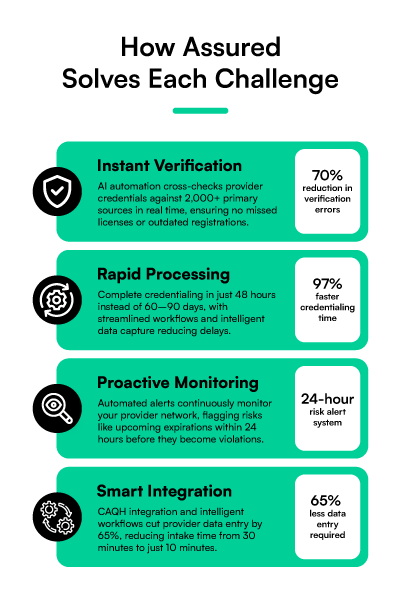
1. Instant Verification for Safety
Assured uses AI automation and technology to cross-check provider credentials against 2,000+ primary sources in real time. This means no missed licenses, outdated DEA registrations, or overlooked sanctions.
Through this process, we have successfully reduced verification errors by 70%, ensuring that only qualified providers treat patients.
2. Rapid Credentialing to Close Care Gaps
With traditional systems, onboarding takes 60 to 90 days. However, with Assured, it takes just 2 days (48 hours). That’s a 97% reduction in credentialing time.
That means new hires are ready to practice within 48 hours, instead of weeks. For CMOs balancing recruitment, service line expansion, and emergency staffing, this level of speed is highly needed.
3. Proactive Compliance Monitoring
Rather than relying on staff to track renewals and deadlines manually, Assured’s automated alerts continues monitoring your provider network, flagging risks like upcoming expirations, missing verifications, or mismatched records within 24 hours.
This way, you are better able to fix problems before they become violations.
4. Provider Readiness with Streamlined Onboarding
Assured doesn’t just ensure an efficient credentialing process, we also streamline provider onboarding, making it simpler and smarter.
Through CAQH integration and intelligent data capture, Assured cuts provider data entry by 65%, decreasing errors and minimizing delays.
Additionally, instead of one-size-fits-all intake forms, Assured creates custom workflows based on provider role, specialty, and location. Providers can complete their intake in just 10 minutes (down from the industry standard of 30).
5. Financial and Scalable Impact
For each delayed specialist, hospitals can lose up to $700,000 in revenue over a 48-day credentialing delay. Across a 300-provider network, that adds up to $1.5–$2 million in annual losses.
Assured helps you recover that revenue and avoid further risk while scaling efficiently. Our platform supports organizations from 10 to 10,000+ providers without performance slowdowns or new compliance gaps.
Quality Metric Impact in Assured's Credentialing: Improving What Matters Most
Below are important metrics that can be improved by using Assured’s efficient credentialing system.
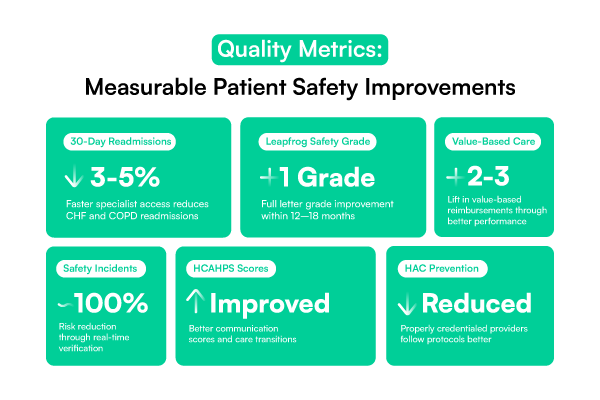
1. Readmission Rate Reduction
When specialists are credentialed quickly, patients get seen sooner. This ensures that appropriate specialists are available for complex cases. Systems using Assured, have reporting seeing 3–5% reductions in 30-day readmissions for conditions like CHF and COPD.
2. Mortality Index Improvement
Assured’s real-time credentialing verification ensures that only qualified providers perform high-risk procedures, which in turn reduces complications and improves your mortality index scores.
3. Hospital-Acquired Condition Prevention
Providers who are properly credentialed are more likely to follow clinical protocols. This leads to measurable reductions in HACs, and a stronger safety culture system-wide.
4. Leapfrog Safety Grade Enhancement
Organizations using automated credentialing systems like Assured often see a full letter grade improvement in Leapfrog scores within 12 to 18 months.
5. Patient Experience Scores
When credentialing delays are eliminated, patients spend less time waiting and more time with the right provider. That improves HCAHPS scores in key areas like "communication with doctors" and "care transitions."
6. Value-Based Care Performance
Many ACO quality measures depend on timely care delivery. Faster onboarding and more accurate provider data translates to better performance and a 2–3% lift in value-based reimbursements.
Real Results: How Assured Strengthens Patient Safety for CMO
Note: Based on 10% of 300 providers delayed 60 days, mitigated by 2-day turnaround
Take Control: Prioritize Patient Safety with Assured
For CMOs, credentialing is the lever that can drive better outcomes, boost quality scores, protect patients, and support long-term financial health. Luckily, Assured makes the credentialing process easier and more efficient.
We deliver what legacy credentialing systems can’t. With Assured, credentialing time reduces from 60–90 days to 48 hours. It cuts $1.5–$2 million in annual losses for 300 providers, reduces compliance risk, improves provider readiness, and supports better care across your system.
If your health system is among the 70% planning to expand by 2025, now is the time to put credentialing at the center of your patient safety strategy.
Book your free Assured consultation today to protect patients, improve quality metrics, and safeguard your reputation!
CMO FAQs: Addressing Your Concerns
How does Assured ensure safety across large networks?
Assured scales to 10,000+ providers. A recent client safely expanded from 600 to 750 providers without disruption.
What’s the implementation timeline?
Just 3 days. Credentialing can begin immediately, with providers approved within 48 hours.
How does it impact our quality metrics?
Clients have seen 3–5% reductions in readmissions, improved Leapfrog grades, and enhanced HCAHPS scores.
How does it improve provider readiness?
Intake takes 10 minutes. Providers enter 65% less data, and get 24-hour support from our team



.png)

