Scaling a healthcare practice from 10 to 200+ providers is exciting growth, but it becomes a credentialing nightmare for teams relying on manual processes and outdated tools. These systems quietly drain time, delay revenue, and create compliance risks that compound as your business grows.
The solution? An automated credentialing system built specifically for growing healthcare practices. Whether you're just starting to expand or already managing multiple provider types across several states, this playbook shows you how to scale efficiently without expanding your administrative team.
The cost of waiting? You could miss out on over $ 500,000 in growth opportunities by 2026.
The Small Practice Credentialing Crisis: Why Manual Processes Fail at Scale
1. The Scale Trap: Industry Data Reveals Hidden Costs of Manual Credentialing
Credentialing is one of the most significant yet often overlooked barriers to growth in healthcare. It looks manageable when you're small, but costs and risks multiply as provider volume increases.
The Financial Reality of Manual Credentialing
The Real Costs:
- Manual credentialing averages $7,500 per provider annually (including time, verification, follow-ups, and error correction)
- For a 50-provider group, that's nearly $375,000 per year
- Credentialing timelines stretch 60-120 days, creating coverage gaps and billing delays
- Specialists lose approximately $8,000 per day while waiting for approvals
The Hidden Expenses Most Practices Miss
Mid-sized practices often patch problems with temporary fixes—hiring consultants, creating workarounds, or adding admin staff just to keep up. Some organizations spend over $175,000 annually compensating for inefficient workflows.
Without automation, these costs quickly spiral out of control. Each new provider increases workload, introduces compliance risks, and strains already overwhelmed staff.
2. The Growth Ceiling Effect: How Manual Systems Create Operational Bottlenecks
Most growing practices hit a wall where manual credentialing becomes unmanageable:
Four Critical Breaking Points for Growing Practices
- Administrative Overload: Staff dedicate up to 23 hours weekly to credentialing tasks, including verifying credentials, compiling documents, tracking renewals, and communicating with payers.
- Staff Burnout: Repetitive manual work kills job satisfaction. High turnover among credentialing coordinators creates knowledge gaps and hinders operational efficiency.
- Compliance Risks: Fatigued staff are more likely to make mistakes. Credentialing files become outdated, licenses lapse unnoticed, and audit responses get delayed. These gaps result in financial penalties exceeding $10,000 per incident.
- Geographic Limitations: Expanding across state lines with manual systems becomes overwhelming. Different requirements, changing regulations, and fragmented tracking make growth risky and slow.
3. Finding the Right Solution: Avoiding the Common Platform Selection Mistakes
Growing practices get stuck between inadequate and overly complex credentialing systems:
The Three Common Platform Traps
- Too Basic—Spreadsheets and Manual Tracking: Fine for under 10 providers, but error-prone and insufficient beyond that. Missed deadlines and incomplete records can result in compliance violations that incur costs of $10,000 or more.
- Too Complex—Enterprise Platforms: Hospital-grade systems require dedicated IT support, extensive integrations, and intensive training. For smaller practices, these become expensive, underutilized frustrations.
- Just Right—Automated, Scalable Tools: Platforms like Assured hit the sweet spot. They automate verification processes, streamline license tracking, and provide compliance oversight without requiring additional staff or IT infrastructure.
The Automation Advantage for Mid-Sized Practices
These solutions reduce manual work by 50% while improving accuracy, and they scale seamlessly as your provider network grows. The key is finding the right balance of functionality and simplicity.
The Three Growth Phases: Identifying Your Current Credentialing Stage and Priorities
Credentialing challenges vary by practice size. Here's how to identify your stage and priorities:
Phase 1: The Spreadsheet Breaking Point for Practices with 10-25 Providers
You're here if:
- Your credentialing coordinator spends 15+ hours weekly updating spreadsheets
- You've missed 1-2 license renewals in the past year
- State expansion feels overwhelming with the current tracking methods
- You're considering hiring a second credentialing person
Immediate Action Items for Phase 1 Practices
Priority: Replace manual tracking before it becomes a compliance liability. Even basic automation delivers immediate ROI.
Quick Wins You Can Expect:
- Cut tracking time from 15 hours to 4 hours weekly
- Eliminate missed renewals with automated alerts
- Expand to 2-3 new states without additional staff
Phase 2: The Growth Bottleneck Stage for Mid-Sized Practices (25-75 Providers)
You're here if:
- You have 2-3 credentialing staff, but still face 60-90 day delays
- Geographic expansion creates compliance complexity
- Payer enrollment backlogs affect revenue
- You're ready to invest in scalable solutions
Strategic Focus for Phase 2 Organizations
Priority: Eliminate workflow inefficiencies and prepare for opportunities to delegate tasks. This is where automation has its greatest impact.
Success Metrics to Track:
- Reduce credentialing time from 82 days to 6 days
- Process 3x more providers with existing staff
- Achieve delegation readiness with major payers
Phase 3: The Coordination Challenge for Large Provider Networks (75+ Providers)
You're here if:
- Multiple departments handle different credentialing aspects
- You manage delegation agreements with 5+ payers
- Audit preparation consumes 200+ staff hours annually
- Manual processes limit strategic growth
Enterprise-Level Goals for Phase 3 Networks
Priority: Centralize coordination and prepare for enterprise-level delegation management. Automation prevents operational chaos.
Enterprise Outcomes to Expect:
- Cut audit prep time by 80%
- Manage unlimited payer relationships efficiently
- Scale to 200+ providers without proportional staff increases
Most practices fall into Phase 2, so we'll focus on examples from this segment, though the principles apply across all phases.
The Cost of Waiting Until 2026: Why Delaying Automation Hurts Growth
The healthcare industry is changing rapidly. Practices that invest in operational efficiency now position themselves to lead, while those that wait fall behind.
Four Market Forces Driving Urgency
- Market Expansion Accelerating: Over 65% of provider organizations plan to grow their networks by 2026. Practices lacking scalable credentialing processes will struggle, not because of talent shortages, but because their administrative operations cannot support expansion.
- Automation Creates Competitive Advantage: Practices using automated credentialing capture 60% more market share than their manual competitors. The speed of provider onboarding directly affects how quickly practices respond to patient demand and payer opportunities.
- Manual Delays Equal Strategic Disadvantage: Traditional credentialing takes 90+ days, putting manual organizations three months behind automated competitors. This delay affects billing, staffing, and patient access across all service lines.
- Missed Expansion Windows: Geographic and service line opportunities have increasingly short windows. Practices with faster credentialing can act quickly when new contracts, locations, or partnerships emerge.
The Compound Cost of Delay: Financial Impact of Postponing Automation
Waiting until 2027 to automate creates cumulative setbacks:
The Four Hidden Costs of Delay
- Revenue Loss: A 50-provider practice loses over $500,000 annually due to delayed onboarding, not counting payer enrollment delays or network participation gaps.
- Rising Technology Costs: Credentialing solutions become more advanced and expensive. Delaying adoption until 2027 could mean paying 15-20% more for the same capabilities.
- Evolving Compliance Requirements: New regulatory demands, particularly from commercial payers, require agile credentialing systems. Manual systems can't adapt quickly, increasing the risk of missed deadlines or outdated documentation.
- Talent Retention Challenges: Staff increasingly prefer tech-enabled environments for credentialing. Repetitive manual processes contribute to burnout, and many coordinators leave for organizations offering modern tools.
Financial Impact Analysis: Calculating ROI for Credentialing Automation
Concrete ROI by Practice Size: Breaking Down the Financial Benefits
Automated credentialing reduces operational spending while maintaining accuracy and compliance.

ROI Analysis by Practice Size
25-Provider Practice:
- Current Manual Cost: $187,500 annually
- With Automation: Up to 75% cost reduction
- Potential Savings: $140,000+ per year
- Break-even: 2-4 months
75-Provider Practice:
- Current Manual Cost: $562,500 annually
- With Automation: Up to 75% cost reduction
- Potential Savings: $420,000+ annually
- Break-even: 2-4 months
150-Provider Practice:
- Current Manual Cost: $1,125,000 annually
- With Automation: Up to 75% cost reduction
- Potential Savings: $840,000+ annually
- Break-even: 2-4 months
Revenue Acceleration Impact: How Faster Credentialing Drives Growth
Manual credentialing averages 82 days from provider hire to approval. Automation cuts this to 6 days.
The Speed Advantage Breakdown
Time Saved: 76 days per provider Impact: Earlier billing and faster patient scheduling Revenue Recovery: $38,000-$152,000 per provider, depending on specialty
For large networks, this improvement translates to millions of dollars in reclaimed revenue annually, without an increase in staff workload.
Risk Mitigation Value: Hidden Benefits of Automated Compliance Management
Automation provides measurable protection against compliance and operational risks with hidden costs:
Three Key Risk Protection Areas
- Penalties Avoided: Late recredentialing, missing verifications, or expired licenses can trigger penalties of $ 10,000 or more. Automation reduces these oversights through real-time tracking and alerts.
- Audit Efficiency: Audit preparation time drops 80% when documentation is standardized and readily accessible.
- Reputation Protection: Public credentialing violations damage trust with patients and payers. Automation helps maintain clean compliance records—an increasingly valuable asset.
Platform Requirements for Small and Mid-Sized Healthcare Practices
Must-Have Features: Essential Capabilities for Successful Credentialing Automation
The Five Essential Platform Capabilities
- Automated Primary Source Verification (PSV): Verifies licenses, certifications, and sanctions directly from authoritative sources. Eliminates 40-50% of manual workload while ensuring regulatory accuracy.
- Multi-State License Tracking: As networks expand across state lines, tracking multiple licensure requirements becomes complex. Built-in tracking prevents compliance violations and ensures continuous readiness.
- Real-Time Monitoring: Alerts you to changes that affect your standing as a provider, so issues are addressed before they become liabilities.
- System Integration: Connects with EMRs, HR platforms, and billing software to eliminate duplicate data entry and improve consistency.
- Scalable Architecture: Grows with your practice, handling increased provider volume, multiple locations, and new payer relationships without requiring process overhauls.
Nice-to-Have Features: Advanced Capabilities That Enhance Operations
Advanced Features for Enhanced Operations
- Advanced Analytics: Dashboards providing visibility into credentialing timelines and staff productivity for data-driven decision-making.
- Custom Workflows: Ability to customize credentialing processes to match your organization's structure and policies.
- White-Label Portals: Custom-branded portals for providers and payers to maintain a professional appearance.
- API Capabilities: Open APIs for advanced customization and tighter integration, valuable for practices with unique software environments.
Integration Requirements: Connecting Your Credentialing Platform with Existing Systems
Seamless integration improves data accuracy, eliminates redundancy, and helps teams work efficiently:
Four Critical Integration Points
- EMR Integration: Ensures provider information consistency across clinical and administrative systems, preventing errors and streamlining scheduling.
- Practice Management Systems: Credentialing data feeds directly into billing systems, ensuring providers connect accurately to payer contracts and reducing reimbursement delays.
- HR Systems: Integration with onboarding platforms initiates credentialing workflows immediately upon hiring providers, thereby avoiding unnecessary delays.
- Communication Tools: Automated updates keep relevant teams informed about credentialing status, outstanding tasks, or urgent issues.
Implementation Strategy: Deploying Automation Without Operational Disruption
The "No-Disruption" Implementation Model
The Three-Phase Implementation Approach
Phase 1: Foundation (1-2 Days)
- System setup reflecting your provider types, workflows, and compliance needs
- Data migration while maintaining current operations (no downtime)
- Core team training (4-6 hours total)
Phase 2: Optimization (Weeks 1-2)
- Workflow customization matching your operations
- Integration activation with EHRs, HR platforms, and payer systems
- Gradual staff transition from manual processing to review and oversight
Phase 3: Full Automation (Weeks 3-4)
- Complete automation of credentialing tasks (verifications, reminders, tracking, committee prep)
- Real-time dashboard monitoring
- Success tracking through key metrics like turnaround time and error rates
Change Management for Small Teams: Supporting Staff Through the Transition
Three Key Areas for Staff Development
- Role Evolution: Staff transitions from data entry to higher-level tasks like quality assurance, reporting, and committee preparation, creating more meaningful work.
- Job Security: Team members assume strategic responsibilities, which enhances satisfaction and mitigates turnover risk.
- Minimal Training: Platforms like Assured require only 6 hours of training, compared to the 40+ hours typically needed for enterprise systems.
Risk Mitigation During Implementation: Protecting Operations Throughout the Transition
Four-Layer Protection Strategy
- Parallel Operation: Your existing process continues uninterrupted until the new system is fully operational and has undergone thorough testing.
- Gradual Migration: Teams adopt the platform in phases, minimizing operational risk and supporting smooth transitions.
- Rollback Capability: Built-in safeguards enable reverting to prior systems if necessary (although most teams don't require this).
- Performance Guarantees: Milestones are tracked with support available at each step to ensure transitions stay on schedule.
Common Implementation Concerns: Addressing the Most Frequent Automation Hesitations
"Are we too small for automation?" - The Scale Question
Automation benefits begin much earlier than most practices realize:
Four Reasons to Start Early
- ROI starts at 10 providers: Even modest teams benefit from reduced admin hours, faster onboarding, and improved accuracy
- Essential beyond 15-20 providers: Without automation, credentialing timelines and staff bandwidth become growth limiters
- Cost per provider decreases with scale: As provider count increases, automation value compounds without requiring additional staff
- Early adoption reduces risk: Implementing before reaching critical volume prevents backlogs and rushed hiring
"Is our current system good enough?" - The Adequacy Question
Manual tracking appears sufficient on the surface, but conceals deeper inefficiencies:
Four Hidden Problems with Manual Systems
- Time consumption: Teams spend 20+ hours weekly managing files, chasing documents, and updating spreadsheets
- Geographic complexity: State expansion adds layers of complexity when handled manually
- Compliance gaps increase: As volume grows, so does the likelihood of missed verifications, expired credentials, and audit exposure
- Talent impact: High admin burden deters candidates and contributes to staff burnout
"Will implementation disrupt operations?" - The Risk Question
Implementation is designed to be fast, supportive, and minimally disruptive:
Four Implementation Safeguards
- Quick setup: Systems typically deploy within 1-2 days without complex configurations
- Parallel operation: Existing processes remain active during rollout, ensuring continuity
- Focused training: Most teams complete onboarding in under six hours
- Dedicated support: You work with a specialist who understands your goals and resolves issues quickly
"How do we justify the investment?" - The ROI Question
Credentialing automation delivers returns across multiple business areas:
Four Areas of Measurable Impact
- Reduced workload: Most teams see a 50%+ reduction in manual credentialing tasks
- Accelerated onboarding: Providers can credential up to 76 days faster, enabling earlier revenue generation
- Lower compliance risk: Real-time monitoring prevents oversights that could lead to $10,000+ penalties
- Growth enablement: Automation removes bottlenecks, allowing network growth without proportional staff increases
Why Choose Assured Over Alternative Credentialing Solutions
Competitive Advantages: What Sets Assured Apart from Other Platforms
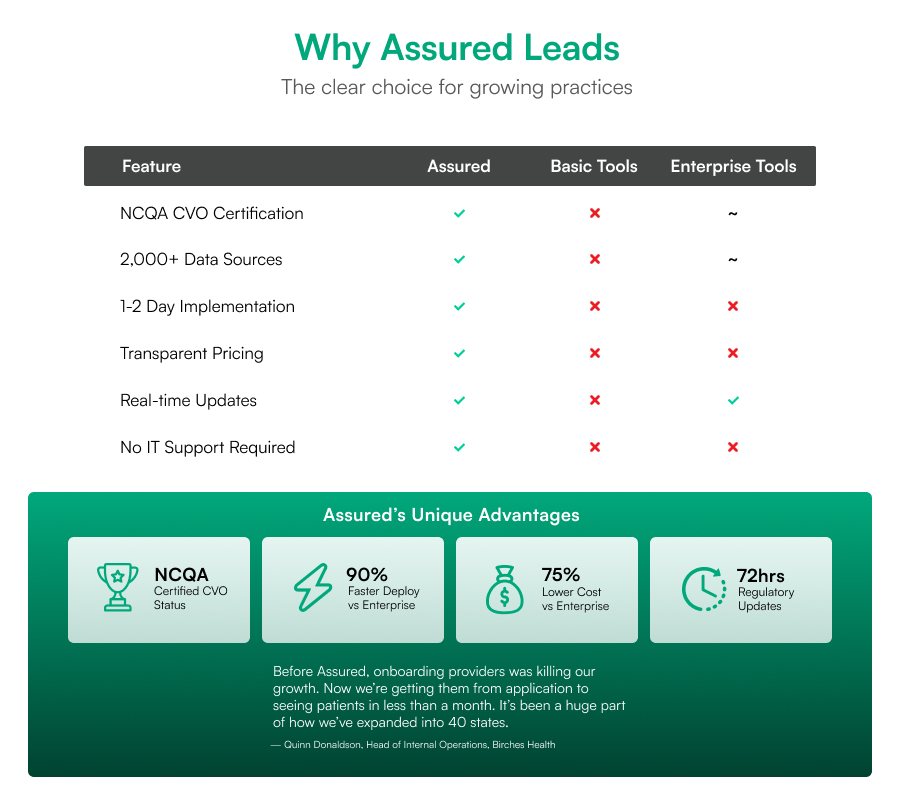
Choosing the right credentialing platform isn't just about features—it's about long-term operational impact and scalability. Assured offers automation, regulatory rigor, and implementation ease specifically for growing healthcare organizations.
Five Key Differentiators for Assured
- NCQA CVO Certification: As a nationally certified Credentials Verification Organization, Assured helps practices meet payer and regulatory expectations with pre-validated processes that reduce audit risk.
- Comprehensive Data Sources: Gathers information from 2,000+ verified sources for thorough, up-to-date primary source verification.
- Rapid Regulatory Updates: Critical regulatory changes are pushed to your platform within 72 hours, keeping teams aligned with evolving standards.
- Fast Implementation: Getting started typically takes 1-2 days on average, with straightforward launch plans tailored to your preferences.
- Transparent Pricing: Simple, upfront pricing with no hidden fees or surprise overages.
Head-to-Head Comparison: Assured vs Enterprise, Basic, and Manual Solutions
Assured vs Enterprise Credentialing Platforms
- 75% lower implementation cost: Eliminates expensive licensing and custom integrations
- 90% faster deployment: Most enterprise solutions require months
- No internal IT support required: Ideal for organizations without large technical teams
Assured vs Basic Credentialing Software
- 3x more functionality: Full lifecycle credentialing, enrollment tracking, license monitoring, automated PSV, and delegation readiness
- Real-time compliance monitoring: Continuously tracks licenses, certifications, and sanctions
- Professional support: Dedicated assistance vs. help desk only
Assured vs Manual Credentialing Processes
- 50%+ time reduction: Automation eliminates repetitive tasks
- 95% error rate reduction: Automated verification prevents mistakes
- Built-in compliance tracking: Real-time alerts and automated reporting vs. manual oversight
Platform Capabilities for Growing Practices: Features Built for Scale
Assured was explicitly built for growing provider groups, offering enterprise-level automation without complexity:
Four Core Platform Capabilities
- AI-Driven Primary Source Verification: Accelerates credentialing by reducing processing times 50% while maintaining accuracy and compliance.
- Intelligent Workflow Management: Prioritizes high-impact tasks based on urgency, provider readiness, and payer timelines to ensure optimal efficiency.
- Multi-State License Coordination: Automatically tracks and manages state-by-state licensing requirements for seamless geographic expansion.
- Real-Time Monitoring and Alerts: Keeps credentialing, enrollment, and compliance data current, helping practices stay ahead of expirations and audits.
- Responsive Support: Every account includes implementation support, rapid response times, hands-on training, and complete documentation.
Customer Success Story: Real Results from Healthcare Organizations
Birches Health Transformation:
"Assured's deep insurance network expertise and bias for action allowed us to open several markets simultaneously, and do so while increasing access to affordable care. Our work with them has helped accelerate growth and been paramount in helping us keep patient and provider experiences high."
— Quinn Donaldson, Head of Internal Operations, Birches Health
Key Outcomes:
- Simultaneous multi-market expansion
- Maintained high patient and provider satisfaction during rapid growth
- Accelerated overall growth trajectory
- Enhanced operational efficiency across markets
This demonstrates how the right credentialing platform enables strategic growth rather than just administrative efficiency.
Decision Framework and Implementation: Your Step-by-Step Guide
Readiness Assessment: Determining If Your Practice Is Ready for Automation
Your practice is prepared for credentialing automation if you meet these criteria:
Five Readiness Indicators
- Provider Volume: Currently managing 10+ providers or expecting to within the next year
- Growth Trajectory: Planning to add at least 5 providers annually through expansion, mergers, or new service lines
- Geographic Reach: Operating across multiple states with coordinated license tracking needs
- Technology Foundation: Using basic practice management software but needing better system integration
- Investment Readiness: Budget allocated for process improvement, prioritizing tools that reduce administrative burden
Vendor Evaluation Checklist: Key Criteria for Platform Selection
Six Essential Evaluation Criteria
- NCQA CVO Certification: Platform should be certified as a Credentials Verification Organization, ensuring recognized standards for accuracy and compliance
- Transparent Pricing: Clear, upfront pricing without hidden costs for better forecasting and vendor relationship management
- Rapid Deployment: Implementation support within 1-2 days for quick results without extensive delays
- System Integration: Seamless compatibility with EMRs, practice management, and HR platforms to reduce data duplication
- Scalability: Capability to support 10x your current provider count without requiring new infrastructure or vendor contracts
- Dedicated Support: Hands-on onboarding, responsive customer support, and ongoing account management
Implementation Timeline and Success Metrics: What to Expect During Deployment
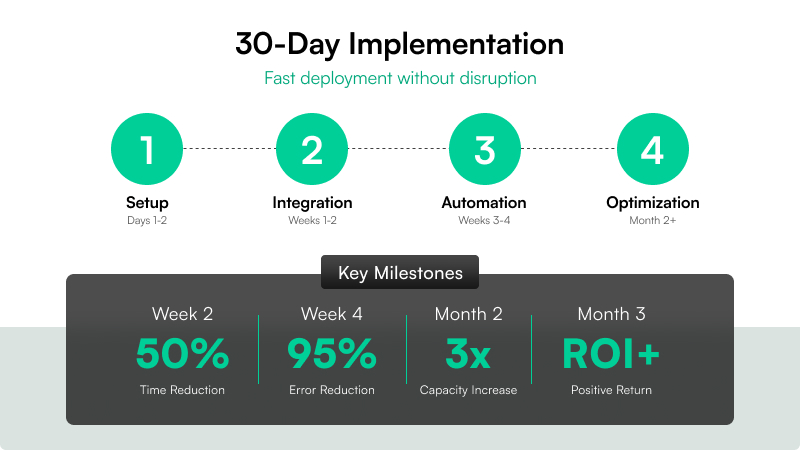
Timeline and Milestone Tracking
Pre-Implementation:
- Vendor selection finalized
- Credentialing goals clarified
- Success metrics identified
- Current state challenges documented
Days 1-2:
- Core setup and data import completed
- Team training finished
- System ready for operation
30-Day Milestone:
- 25% reduction in credentialing turnaround time
- Fewer backlogs and faster intake
- Cleaner application files
60-Day Milestone:
- 40% reduction in credentialing-related administrative workload
- Less time chasing documents or tracking statuses manually
90-Day Milestone:
- Full ROI achieved
- Scalable credentialing capability established for future growth
Performance Guarantees: How Assured Ensures Your Success
Assured delivers measurable outcomes:
Three Performance Commitments
- Time Savings Guarantee: If you don't achieve at least a 50% reduction in credentialing workload, we provide refunds or extended support
- Compliance Protection: System configured to prevent regulatory violations or missed deadlines during implementation, with audit-ready documentation
- Full Integration Promise: Your EMRs, HR tools, and payer enrollment processes integrate with Assured within 30 days
Conclusion
For small and mid-sized healthcare organizations, scaling efficiently without expanding administrative headcount is both a competitive advantage and an operational necessity.
The right time to modernize credentialing is before growth overwhelms your current system. Whether you're managing 10 providers today or preparing to cross 100, the financial, compliance, and operational risks of manual processes only increase with scale.
Why Assured Is the Right Choice
Assured offers a practical, proven solution built specifically for practices like yours. With automated workflows, NCQA-certified verification, and rapid implementation, Assured helps you reduce credentialing time by up to 95%, eliminate administrative bottlenecks, and stay compliant across multiple states and payer networks.
You don't need a larger team to grow. You need better infrastructure.


.jpg)
.png)


.png)